You are here: Home > Medical Countermeasures Database > Ibuprofen
Ibuprofen - Medical Countermeasures Database
- Name of Chemical Defense therapeutic agent/device
- Chemical Defense therapeutic area
- Evidence-based medicine for Chemical Defense
- Pharmacokinetic and toxicokinetics data
- Indication/dosing
- Formulation/shelf life
- Off-label use & dosing
- Route of administrating/monitoring
- Adverse effects
- Contraindications
- Clinical studies in progress
- Non-clinical studies in progress
- Needed studies for Chemical Defense
- Needed studies for non-Chemical Defense
- Study-related ethical concerns
- Global regulatory status
- Other potentially useful information
- Publications
- Web sites
1. Name of Chemical Defense therapeutic agent/device
Ibuprofen
2. Chemical Defense therapeutic area(s)
— including key possible usesIbuprofen has been shown in vitro to inhibit phosgene-increased IL-8 inflammatory cytokine production associated with neutrophil infiltration of the lung linked with the onset and progression of acute lung injury. It has also improved survival rate in animal models after phosgene exposure.
3. Evidence-based medicine for Chemical Defense
— including efficacy and safetyA. Summary
Structure
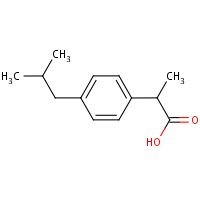
HSDB. Ibuprofen
Mechanism of action
-
Ibuprofen has pharmacologic actions similar to those of other prototypical NSAIAs. Ibuprofen has shown anti-inflammatory, antipyretic, and analgesic activity in both animals and humans. The exact mechanisms of action of the drug have not been clearly established, but many of the actions appear to be associated principally with the inhibition of prostaglandin synthesis. Ibuprofen inhibits synthesis of prostaglandins in body tissues by inhibiting cyclooxygenase; at least 2 isoenzymes, cyclooxygenase-1 (COX-1) and -2 (COX-2) (also referred to as prostaglandin G/H synthase-1 [PGHS-1] and -2 [PGHS-2], respectively), have been identified that catalyze the formation of prostaglandins in the arachidonic acid pathway. Ibuprofen, like other prototypical NSAIAs, inhibits both COX-1 and COX-2. Although the exact mechanisms have not been clearly established, NSAIAs appear to exert anti-inflammatory, analgesic, and antipyretic activity principally through inhibition of the COX-2 isoenzyme; COX-1 inhibition presumably is responsible for the drugs' unwanted effects on GI mucosa and platelet aggregation.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
Summary of clinical and non-clinical studies
Phosgene (carbonyl chloride) is a volatile and highly toxic acid chloride that poses a potential bioterrorism threat due to the ease and low expense of production (Sciuto and Hurt, 2004). It also may arise as a product of industrial/occupational accidents, and there is a risk of low level environmental exposure. It is a highly reactive tissue oxidant which destroys a wide range of cellular macromolecules and precipitates the release of inflammatory cytokines, eventually resulting in weakening and collapse of the blood-air barrier and a subsequent flooding of the lungs (Borak and Diller, 2001). Mortality therefore occurs as a result of a delayed, but serious, fulminating pulmonary edema arising 2-24 hours after exposure. Ibuprofen protects against phosgene-induced lung injury, possibly by forming iron complexes and preventing the iron-mediated generation of oxidants (Kennedy et al., 1990). Human lung cell cultures produce high levels of the inflammatory cytokine IL-8 upon phosgene exposure; these levels were reduced by approximately 50% after treatment with ibuprofen (Cowan et al., 2005). Ibuprofen injected into male mice within 20 minutes after phosgene exposure, and again 5 hours after exposure, resulted in significantly higher 12-hour survival rates (Sciuto and Hurt, 2004). Rats receiving ibuprofen 30 minutes before and 1 hour after phosgene exposure showed a significantly lower lung wet weight due to reduced edema (Sciuto et al., 1996). Based on data from animal models, at least 25-50 mg/kg oral ibuprofen would be required to achieve a plasma drug concentration that may be effective against phosgene (Borak and Diller, 2001). No confirmatory human clinical data is available.
B. Link to clinical studies
Pregnancy, breastfeeding studies
-
A 2006 case-control study found a significant association between congenital anomalies, specifically cardiac septal defects, and the use of NSAIDs in the 1st trimester. A population-based pregnancy registry (N = 36,387) was developed by linking three databases in Quebec. Case infants were those with any congenital anomaly diagnosed in the first year of life and were compared with matched controls. There were 93 infants (8.8%) with congenital defects from 1056 mothers who had filled prescriptions for NSAIDs in the 1st trimester. In controls, there were 2478 infants (7%) with anomalies from 35,331 mothers who had not filled such a prescription. The adjusted OR was 2.21 (95% CI 1.72-2.85). The adjusted OR for cardiac septal closure was 3.34 (95% CI 1 .87-5.98). There also was a significant association for anomalies of the respiratory system 9.55 (95% CI 3.08-29.63), but this association disappeared when cases coded as "unspecified anomaly of the respiratory system" were excluded. For the cases involving septal closure, 61 % were atrial septal defects and 31 % were ventricular septal defects. There were no significant associations for oral clefts or defects involving other major organ systems. The five most common NSAIDs were naproxen (35%), ibuprofen (26%), rofecoxib (15%), diclofenac (9%), and celecoxib (9%). Among these agents, the only significant association was for ibuprofen prescriptions in the 1st trimester and congenital defects (p <0.01) (Class III).
Briggs GG, Freeman RK, Yaffe SJ, eds.: Drugs in Pregnancy and Lactation, Ninth Edition. Lippincott Williams & Wilkins, Philadelphia, PA 2008 p.714-716
-
A combined 2001 population-based observational cohort study and a case-control study estimated the risk of adverse pregnancy outcome from the use of NSAIDS. The studies were based on data from the Danish Birth Registry and the North Jutland County's hospital discharge registry collected between 1991 and 1998. Only those women who had received a prescription for a NSAID at doses equivalent to 400 or 600 mg of ibuprofen were classified as exposed (NSAID doses equivalent to 200 mg of ibuprofen are over-the-counter in Denmark). The cohort involved 1462 pregnant women who had received a NSAID prescription in the interval from 30 days before conception to birth and a reference group of 17,259 pregnant women who had not been prescribed any drugs during pregnancy. In both groups, only pregnancies lasting >28 weeks' were included. There were 1106 women (76%) who had received a NSAID prescription between 30 days before conception and the end of the 1st trimester. The prevalence of congenital malformations in infants of these women and the reference group were (N = 46, 4.2%, 95% confidence interval [CI] 3.0%-5.3% vs. N = 564, 3.3%, 95% CI 3.0%-3.5%), respectively; adjusted odds ratio (OR) 1.27 (95% CI 0.93-1 .75). A total of 997 women received a NSAID prescription in the 2nd and/or 3rd trimesters. In this group, the OR for preterm delivery was 1.05 (95% CI 0.80-1 .39) and that for low birth weight (excluding preterm infants) was 0.79 (95% CI 0.45-1 .38). Adjusting the data for the use of indomethacin (the tocolytic of choice in Denmark) did not affect the results. There was no evidence of a specific grouping of defects or of a dose-response relationship for adverse birth outcome. Based on the analysis, the authors concluded that NSAIDS were not associated with adverse birth outcome (Class III).
Briggs GG, Freeman RK, Yaffe SJ, eds.: Drugs in Pregnancy and Lactation, Ninth Edition. Lippincott Williams & Wilkins, Philadelphia, PA 2008 p.714-716
-
A 1996 case-control study of gastroschisis found a significantly elevated risk for ibuprofen (N = 6; OR 4.0, 95% CI 1 .0-16.0) and other medications and exposures. A significant association was also found for aspirin (N = 7; OR 4.67, 95% CI 1.21-18.05). The data supported a vascular hypothesis for the pathogenesis of gastroschisis (Class III).
Briggs GG, Freeman RK, Yaffe SJ, eds.: Drugs in Pregnancy and Lactation, Ninth Edition. Lippincott Williams & Wilkins, Philadelphia, PA 2008 p.714-716
-
Ibuprofen is excreted into human milk. Two studies were unable to detect the drug (19-21), but a third study using a more sensitive assay (lower limit 2.5 ng/mL) was able to quantify ibuprofen in milk. In 12 patients taking 400 mg every 6 hours for 24 hours, an assay capable of detecting 1 mcg/mL failed to demonstrate Ibuprofen in the milk. In a second report, a woman was treated with 400 mg twice daily for 3 weeks. Milk levels shortly before and up to 8 hours after drug administration were all <0.5 mcg/mL. The third study involved a lactating woman who underwent maxillary surgery. After surgery, she took ibuprofen (400 mg) six times over a 42.5-hour interval for postoperative pain. Ten breast milk samples were collected during this same period. Ibuprofen was detected (13 ng/mL) 30 minutes after the first dose. The maximum milk concentration (181 ng/mL) was found 20.5 hours after the first dose (about 5 hours after the third dose). Although the infant was not nursing, the infant's weight adjusted dose would have been an estimated 0.0008% of the mother's dose (Class III).
Briggs GG, Freeman RK, Yaffe SJ, eds.: Drugs in Pregnancy and Lactation, Ninth Edition. Lippincott Williams & Wilkins, Philadelphia, PA 2008 p.714-716
Clinical reviews
-
Phosgene (carbonyl chloride, CAS 75-44-5) is a highly reactive gas of historical interest and current industrial importance. Phosgene has also proved to be a useful model for the study of those biochemical mechanisms that lead to permeability-type pulmonary edema (adult respiratory distress syndrome). In turn, the study of phosgene-induced adult respiratory distress syndrome has provided insights leading to revised treatment strategies for exposure victims. We summarized recent findings on the mechanisms of phosgene-induced pulmonary edema and their implications for victim management. In light of that research, we also provide a comprehensive approach to the management and treatment of phosgene exposure victims (Class IV).
Borak J, Diller WF; Phosgene exposure: mechanisms of injury and treatment strategies. J Occup Environ Med 2001; 43 (2): 110-9. [PubMed Citation]
C. Link to non-clinical (e.g., animal) studies
Adult animal studies
-
A series of studies was performed to address treatment against the former chemical warfare edemagenic gas phosgene. Both in situ and in vivo models were used to assess the efficacy of postexposure treatment of phosgene-induced lung injury using clinically existing drugs. The degree of efficacy was judged by examining treatment effects on pulmonary edema formation (PEF) as measured by wet/dry weight (WW/DW) ratios, real-time (in situ) lung weight gain (LWG), survival rates (SR), odds ratios, and glutathione (GSH) redox states. Drugs included N-acetylcysteine (NAC), ibuprofen (IBU), aminophylline (AMIN), and isoproterenol (ISO). Using the in situ isolated perfused rabbit lung model (IPRLM), intratracheal (IT) NAC (40 mg/kg bolus) delivered 45-60 min after phosgene exposure (650 mg/m(3)) for 10 min lowered pulmonary artery pressure, LWG, leukotrienes (LT) C(4)/D(4)/E(4), lipid peroxidation, and oxidized GSH. We concluded that NAC protected against phosgene-induced lung injury by acting as an antioxidant by maintaining protective levels of GSH, reducing both lipid peroxidation and production of arachidonic acid metabolites. Also in IPRLM, administration of AMIN (30 mg/kg) 80-90 min after phosgene exposure significantly reduced lipid peroxidation and perfusate LTC(4)/D(4)/E(4), reduced LWG, and prevented phosgene-induced decreases in lung tissue cAMP. These data suggest that protective mechanisms observed with AMIN involve decreased LTC(4)/D(4)/E(4) mediated pulmonary capillary permeability and attenuated lipid peroxidation. Direct antipermeability effects of AMIN-induced upregulation of cAMP on cellular contraction may also be important in protection against phosgene-induced lung injury. Posttreatment with ISO in the IPRLM by either combined intravascular (iv; infused into pulmonary artery at 24 microg/min infused) + IT (24 microg bolus) or IT route alone 50-60 min after phosgene exposure significantly lowered pulmonary artery pressure, tracheal pressure, and LWG. ISO treatment significantly enhanced GSH products or maintained protective levels when compared with results from phosgene-exposed only rabbits. These data suggest that protective mechanisms for ISO involve reduction in vascular pressure, decreased LTC(4)/D(4)/E(4)-mediated pulmonary capillary permeability, and favorably maintained lung tissue GSH redox states. For in vivo male mouse (CD-1, 25-30 g) studies IBU was administered ip within 20 min after a lethal dose of phosgene (32 mg/m(3) for 20 min) at 0 (saline), 3, 9, or 15 mg/mouse. Five hours later, a second IBU injection was given but at half the original doses (0, 1.5, 4.5, and 7.5 mg/mouse); therefore, these treatment groups are now referred to as the 0/0, 3/1.5, 9/4.5, and 15/7.5 mg IBU/mouse groups. SRs and odds ratios were calculated for each dose at 12 and 24 h. The 12-h survival was 63% for 9/4.5 mg IBU and 82% for the 15/7.5 mg IBU groups, compared with 25% for saline-treated phosgene-exposed mice. At 24 h, those survival rates were reduced to 19%, 19%, and 6%, respectively. In the 15/7.5 mg IBU group, lung WW/DW ratios were significantly lower than in saline-treated mice at 12 h. Lipid peroxidation was lower only for the 9/4.5 mg IBU dose; however, nonprotein sulfhydryls (a measure of GSH) were greater across all IBU doses. The odds ratio was 5 for the 9/4.5 IBU group at 12 h and 13 for the 15/7.5 mg IBU group, compared with 3.5 for both groups at 24 h. IBU posttreatment increased the survival of mice at 12 h by reducing PEF, lipid peroxidation, and GSH depletion. In conclusion, effective treatment of phosgene-induced lung injury involves early postexposure intervention that could reduce free radical species responsible for lipid peroxidation, correct the imbalance in the GSH redox state, and prevent the release of biological mediators such as leukotrienes, which are accountable for increased permeability.
Sciuto AM, Hurt HH; Therapeutic treatments of phosgene-induced lung injury. Inhalation Toxicology 2004; 16 (8): 565-80. [PubMed Citation]
-
Phosgene, a highly reactive former warfare gas, is a deep lung irritant which produces adult respiratory distress syndrome (ARDS)-like symptoms following inhalation. Death caused by phosgene involves a latent, 6-24-h, fulminating non-cardiogenic pulmonary edema. The following dose-ranging study was designed to determine the efficacy of a non-steroidal anti-inflammatory drug, ibuprofen (IBU), and a methylxanthine, pentoxifylline (PTX). These drugs were tested singly and in combination to treat phosgene-induced acute lung injury in rats. Ibuprofen, in concentrations of 15-300 mg kg-1 (i.p.), was administered to rats 30 min before and 1 h after the start of whole-body exposure to phosgene (80 mg m-3 for 20 min). Pentoxifylline, 10-120 mg kg-1 (i.p.), was first administered 15 min prior to phosgene exposure and twice more at 45 and 105 min after the start of exposure. Five hours after phosgene inhalation, rats were euthanized, the lungs were removed and wet weight values were determined gravimetrically. Ibuprofen administered alone significantly decreased lung wet weight to body weight ratios compared with controls (P < or = 0.01) whereas PTX, at all doses tested alone, did not. In addition, the decrease in lung wet weight to body weight ratio observed with IBU+PTX could be attributed entirely to the dose of IBU employed. This is the first study to show that pre- and post-treatment with IBU can significantly reduce lung edema in rats exposed to phosgene.
Sciuto AM et al; Efficacy of ibuprofen and pentoxifylline in the treatment of phosgene-induced acute lung injury. J Appl Toxicol 1996; 16 (5): 381-4 (1996) [PubMed Citation]
-
Because ibuprofen protects from septic lung injury, we studied the effect of ibuprofen in oxidant lung injury from phosgene. Lungs from rabbits exposed to 2,000 ppm-min phosgene were perfused with Krebs-Henseleit buffer at 50 ml/min for 60 min. Phosgene caused no increase in lung generation of cyclooxygenase metabolites and no elevation in pulmonary arterial pressure, but markedly increased transvascular fluid flux (delta W = 31 +/- 5 phosgene vs. 8 +/- 1 g unexposed, P less than 0.001), permeability to albumin (125I-HSA) lung leak index 0.274 +/- 0.035 phosgene vs. 0.019 +/- 0.001 unexposed, P less than 0.01; 125I-HSA lavage leak index 0.352 +/- 0.073 phosgene vs. 0.008 +/- 0.001 unexposed, P less than 0.01), and lung malondialdehyde (50 +/- 7 phosgene vs. 24 +/- 0.7 mumol/g dry lung unexposed, P less than 0.01). Ibuprofen protected lungs from phosgene (delta W = 10 +/- 2 g; lung leak index 0.095 +/- 0.013; lavage leak index 0.052 +/- 0.013; and malondialdehyde 16 +/- 3 mumol/g dry lung, P less than 0.01). Because iron-treated ibuprofen failed to protect, we studied the effect of ibuprofen in several iron-mediated reactions in vitro. Ibuprofen attenuated generation of hydroxyl radicals by a Fenton reaction and peroxidation of arachidonic acid by FeCl3 and ascorbate. Ibuprofen also formed iron chelates that lack the free coordination site required for iron to be reactive. Thus, ibuprofen may prevent iron-mediated generation of oxidants or iron-mediated lipid peroxidation after phosgene exposure. This suggests a new mechanism for ibuprofen's action.
Kennedy TP et al; Ibuprofen prevents oxidant lung injury and in vitro lipid peroxidation by chelating iron. J Clin Invest. 1990; 86 (5): 1565-73 (1990) [PubMed Citation]
Other non-clinical studies
Human non-clinical studies-
Inflammation and edema are associated with respiratory and cutaneous exposure to sulfur mustard (SM) as well as with phosgene-induced lung injury. IL-8 is a key inflammatory cytokine that recruits neutrophils linked with the onset and progression of acute lung injury caused by inhalation of these chemical agents. In the present study, human lung small airway cell (SAC) cultures were exposed to either SM [25 to 400 uM] or phosgene [0.1 to 6.4 ppm. min]. IL-8 was increased after exposure to either SM or phosgene. At the optimum exposures for SM (100 uM) and phosgene (1.6 ppm.min), IL-8 was increased by 1013 +/-123 pg/ml and 965 +/-181 pg/ml, respectively. Higher exposures to either agent increased cytotoxicity and decreased IL-8 levels. Ibuprofen has shown efficacy against phosgene pulmonary toxicity in mice. Ibuprofen (62, 125, 250, 500, 1000 uM) significantly diminished phosgene-increased IL-8 in SAC cultures exposed to 2 ppm.min phosgene. Maximum inhibition of nearly 50% of phosgene-increased IL-8 was seen at 125 and 250 uM doses of ibuprofen (from 1141 +/-143 pg/ml to 628 +/-105, 593 +/-69 pg/ml respectively). Chemical insult-increased IL-8 in SAC cultures provides an assay for screening countermeasures against the inhalation toxicity of chemical threat agents. The increase in the inflammatory cytokine IL-8 by both SM and phosgene may further provide common pharmacological targets for drugs with Multi-Threat Medical Countermeasure (MTMC) action against distinct chemical threats.
Cowan FM, Smith WJ et al.; Sulfur Mustard- And Phosgene- Increased IL-8 In Human Small Airway Cell Cultures: Implications For Medical Countermeasures Against Inhalation Toxicity. Proceedings of the U.S. Army Medical Defense Bioscience Review. (2005). [PubMed Citation]
4. Pharmacokinetic and toxicokinetics data
— including children-, pregnancy-, geriatric-, and obesity-related dataAdult
-
Approximately 80% of an oral dose of ibuprofen is absorbed from the GI tract. Absorption rate is slower and plasma concentrations are reduced when ibuprofen tablets, chewable tablets, or suspension are taken with food; however, the extent of absorption is not affected. When the drug is administered with food, peak plasma ibuprofen concentrations are reduced by 30-50% and time to achieve peak plasma concentrations is delayed by 30-60 minutes.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
In adults, oral bioavailability of ibuprofen (measured by peak plasma concentrations and extent of absorption) is similar following administration of conventional tablets, chewable tablets, or suspension; however, time to reach peak plasma concentrations was reportedly about 120, 62, or 47 minutes following administration of each respective dosage form.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Following oral administration of a single 200-mg dose of ibuprofen as chewable tablets, suspension, or conventional tablets in adults, peak plasma concentrations were 15, 19, or 20 mcg/mL, respectively. Following oral administration of ibuprofen in adults, the area under the serum concentration-time curves (AUCs) of total and free drug increase proportionally with single ibuprofen doses of 50-600 and up to 1200 mg, respectively.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Ibuprofen is metabolized via oxidation to form 2 inactive metabolites, (+)-2[4'-(2-hydroxy-2-methylpropyl)phenyl]propionic acid (metabolite A) and (+)-2-[4'-(2-carboxypropyl)phenyl]propionic acid (metabolite B). About 50-60% of an oral dose is excreted in urine as metabolites A and B or their glucuronide conjugates within 24 hours. Less than 10% of the drug is excreted in urine unchanged; the remainder of the drug is eliminated in feces, both as metabolites and unabsorbed drug.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
Children
-
In febrile children, oral bioavailability (measured by peak plasma concentrations and extent of absorption) of ibuprofen also appears to be similar following administration of the respective dosage form; however, time to reach peak plasma concentrations was reportedly 86 or 58 minutes following administration of chewable tablets or suspension, respectively.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Following oral administration of a 10-mg/kg dose in febrile children, peak plasma concentrations and plasma concentration-time curves (AUCs) of ibuprofen appear to be increased in children compared with those achieved in adults; these differences appear to result from age- or fever-related changes in the volume of distribution in children and also to the variability of doses (based on body weight) administered to pediatric patients. Peak plasma or serum ibuprofen concentrations of about 40-55 mcg/mL occur after about 1-1.5 hours in febrile children receiving a single 10-mg/kg dose of ibuprofen suspension or chewable tablets. Following oral administration of ibuprofen suspension in febrile children, AUCs increase with increasing single ibuprofen doses up to 10 mg/kg; it appears that pharmacokinetics of ibuprofen are not affected by age, in children 2 to 11 years of age.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
The elimination, disposition and protein binding of ibuprofen (IBU) in premature infants were studied for use in the prevention of intraventricular hemorrhage and closure of patent ductus arteriosus. The kinetic profile of i.v. IBU lysine (10 mg/kg bolus) given within the first 3 h after birth was studied in 21 premature neonates (mean birth weight = 944.7 g, range: 575-1450 g; gestational age: 26.8 weeks, range: 22-31 weeks). Blood samples (0.3 ml/sample) were obtained at time 0 and at 1, 3, 6, 12, 24, 48, and 72 h post-dose for IBU by high-performance liquid chromatography (HPLC). Kinetic analyses assumed applicability of one open-compartment model and calculations from the model-independent areas under the time concentration curve (AUC). Data (mean +/- SEM) show that apparent volume of distribution (AVd) was 62.1 +/- 3.9 ml/kg, plasma t1/2 beta was 30.5 +/- 4.2 h, elimination rate constant (Kel) was 0.032 +/- 0.004 h-1, plasma clearance was 2.06 +/- 0.33 ml/kg/h and plasma concentration (Cp) at 1 h was 180.6 +/- 11.1 mg/l. Gestational age and birth weight were not related to drug elimination. In 10 neonates, IBU maintenance dose of 5 mg/kg once daily on days 2 and 3 generated mean Cp of 116.6 +/- 54.5 mg/l and 113.6 +/- 58.2 mg/l, respectively. Protein binding by ultrafiltration and capillary electrophoresis showed that the percentage bound IBU was significantly lower in full term cord plasma (94.98 +/- 0.39%, n = 26) compared to adult plasma protein (mean +/- SE = 98.73 +/- 0.31%, n = 8, p < 0.0001). Compared to data from adults and older children, IBU elimination is markedly prolonged in neonates and protein binding is slightly lower. Thus, investigational and clinical therapeutic regimens should be adjusted to account for decreased drug disposition to ensure safe and effective therapy.
Aranda JV, Varvarigou A, Beharry K, Bansal R, Bardin C, Modanlou H, Papageorgiou A, Chemtob S; Pharmacokinetics and protein binding of intravenous ibuprofen in the premature newborn infant. Acta Paediatr. 1997 Mar; 86 (3): 289-93.[PubMed Citation]
Geriatric
-
By using stable isotope methodology, we studied the disposition of ibuprofen after the first and last dose of a 4-week regimen of 800 mg of racemic ibuprofen every 8 hr in three groups of subjects: 1) young healthy volunteers (n = 8); 2) healthy elderly volunteers (n = 14); and 3) elderly patients with creatinine clearance between 30 and 70 ml/min (n = 13). Stereoselective gas chromatography-mass spectrometry was used to quantify deuterated S- and nondeuterated R- and S-ibuprofen in serum up to 24 hr after the first and last doses. Urinary excretion of the stereoisomeric forms of carboxyibuprofen, hydroxyibuprofen and ibuprofen glucuronide were determined up to 24-hr postdose by stereoselective high-performance liquid chromatography. Stereoselective serum protein binding was determined by ultrafiltration. Both elderly groups had significantly decreased binding of S-ibuprofen compared to the young group. The S-ibuprofen pharmacokinetics were significantly different in the elderly patients with renal impairment compared to the young volunteers: the T1/2 was increased, the unbound clearance was decreased and the unbound concentration at steady state was increased. Fraction inverted was similar for all groups, but unbound clearances of glucuronidation and hydroxylation were reduced in the elderly patients with renal impairment. These results suggest that the disposition of ibuprofen enantiomers is altered in elderly persons with renal impairment; these changes may increase the risk for nonsteroidal anti-inflammatory drug-associated adverse effects in such patients.
Rudy AC, Knight PM, Brater DC, Hall SD; Enantioselective disposition of ibuprofen in elderly persons with and without renal impairment. J Pharmacol Exp Ther. 1995 Apr; 273 (1):88-93. [PubMed Citation]
5. Current FDA/EUA approved indications and dosing
— including children-, pregnancy-, geriatric-, and obesity-related data, and Emergency Use Authorization (EUA)Adults (FDA)
-
Rheumatoid arthritis and osteoarthritis: the usual adult oral dosage of ibuprofen in the symptomatic treatment of acute and chronic rheumatoid arthritis and osteoarthritis is 400-800 mg 3 or 4 times daily. Dosage should be adjusted according to the response and tolerance of the patient and should not exceed 3.2 g daily.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Mild to moderate pain: the usual adult oral dosage of ibuprofen is 400 mg every 4-6 hours as necessary. Alternatively, for self-medication of mild to moderate pain, the usual initial adult dosage is 200 mg every 4-6 hours; dosage may be increased to 400 mg every 4-6 hours if pain does not respond to the lower dosage but should not exceed 1.2 g daily unless directed by a clinician.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Self-medication of migraine pain: the usual adult dosage of ibuprofen liquid-filled capsules is 400 mg ... Doses greater than 400 mg have not provided a greater analgesic effect than the 400-mg dose.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Pain: individuals 17 years of age or older may receive ibuprofen in a dosage of 400-800 mg IV every 6 hours as needed; ibuprofen dosage should not exceed 3.2 g in a 24-hour period.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Primary dysmenorrheal: ibuprofen therapy should be started with the earliest onset of pain; the usual adult oral dosage in these patients is 400 mg every 4 hours as necessary for relief of pain. Alternatively, for self-medication of dysmenorrhea, the usual initial adult dosage is 200 mg every 4-6 hours; dosage may be increased to 400 mg every 4-6 hours if necessary but should not exceed 1.2 g daily unless otherwise directed by a clinician.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Self-medication of fever: the usual initial adult dosage of ibuprofen is 200 mg every 4-6 hours; dosage may be increased to 400 mg every 4-6 hours if fever is not adequately reduced at the lower dosage but should not exceed 1.2 g daily unless otherwise directed by a clinician.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Fever: individuals 17 years of age or older may receive an initial dose of ibuprofen 400 mg IV followed by 400 mg IV every 4-6 hours or 100-200 mg IV every 4 hours. Ibuprofen dosage should not exceed 3.2 g in a 24-hour period.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
Children (FDA)
-
Juvenile rheumatoid arthritis: the recommended ibuprofen oral dosage is 30-40 mg/kg daily divided into 3 or 4 doses. An ibuprofen dosage of 20 mg/kg daily in divided doses may be adequate for children with mild disease. Dosages exceeding 50 mg/kg daily are not recommended in children with juvenile arthritis, since such dosages have not been studied. In addition, dosages exceeding 40 mg/kg daily may increase the risk of drug-induced adverse effects.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Mild to moderate pain: in children 6 months to 12 years of age, the recommended ibuprofen oral dosage is 10 mg/kg every 6-8 hours; the maximum dosage of ibuprofen is 40 mg/kg daily. For self-medication of minor aches and pains in pediatric patients, ibuprofen dosages should be calculated based on body weight rather than age whenever possible.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Dose adjustment: infants 6-11 months of age or those weighing 12-17 pounds (approximately 5-8 kg) may receive 50 mg of ibuprofen, infants 12-23 months of age or those weighing 18-23 pounds (approximately 8-10 kg) may receive 75 mg, children 2-3 years of age or those weighing 24-35 pounds (approximately 11-16 kg) may receive 100 mg, children 4-5 years of age or those weighing 36-47 pounds (approximately 16-21 kg) may receive 150 mg, children 6-8 years of age or those weighing 48-59 pounds (approximately 22-27 kg) may receive 200 mg, children 9-10 years of age or those weighing 60-71 pounds (approximately 27-32 kg) may receive 250 mg, and children 11 years of age or those weighing 72-95 pounds (approximately 33-43 kg) may receive 300 mg; these doses may be administered every 6-8 hours and no more than 4 times daily.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Antipyresis: in children 6 months to 12 years of age, the usual oral dosage of ibuprofen is 5 or 10 mg/kg for temperatures below or above 39°C, respectively. The maximum daily dosage of ibuprofen in febrile children is 40 mg/kg.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Self-medication of fever: in pediatric patients, ibuprofen dosages should be calculated based on body weight rather than age whenever possible. Infants 6-11 months of age or those weighing 12-17 pounds (approximately 5-8 kg) may receive 50 mg of ibuprofen, infants 12-23 months of age or those weighing 18-23 pounds (approximately 8-10 kg) may receive 75 mg, children 2-3 years of age or those weighing 24-35 pounds (approximately 11-16 kg) may receive 100 mg, children 4-5 years of age or those weighing 36-47 pounds (approximately 16-21 kg) may receive 150 mg, children 6-8 years of age or those weighing 48-59 pounds (approximately 22-27 kg) may receive 200 mg, children 9-10 years of age or those weighing 60-71 pounds (approximately 27-32 kg) may receive 250 mg, and children 11 years of age or those weighing 72-95 pounds (approximately 33-43 kg) may receive 300 mg; these doses may be administered every 6-8 hours and no more than 4 times daily.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Patent ductus arteriosus (PDA): in premature neonates, ibuprofen lysine is administered by IV infusion over 15 minutes. A course of therapy consists of 3 doses of ibuprofen lysine administered at 24-hour intervals. All doses are based on the neonate's birth weight. The first IV dose of ibuprofen in the course is 10 mg/kg; the second and third doses are 5 mg/kg each, administered 24 and 48 hours after the first dose.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
Pregnancy (FDA)
FDA Pregnancy Risk Category:
-
C; RISK CANNOT BE RULED OUT. Adequate, well controlled human studies are lacking, and animal studies have shown risk to the fetus or are lacking as well. There is a chance of fetal harm if the drug is given during pregnancy; but the potential benefits may outweigh the potential risk.(prior to 30 weeks gestation)
-
D; POSITIVE EVIDENCE OF RISK. Studies in humans, or investigational or post-marketing data, have demonstrated fetal risk. Nevertheless, potential benefits from the use of the drug may outweigh the potential risk. For example, the drug may be acceptable if needed in a life-threatening situation or serious disease for which safer drugs cannot be used or are ineffective. (starting at 30 weeks to gestation)
Product label CALDOLOR (ibuprofen) injection [Cumberland Pharmaceuticals Inc.] Last revised: June 2009 [DailyMed]
Nursing Mothers (FDA)
Lactation Risk Category:
-
L1 Safest; Drug which has been taken by a large number of breastfeeding mothers without any observed increase in adverse effects in the infant. Controlled studies in breastfeeding women fail to demonstrate a risk to the infant and the possibility of harm to the breastfeeding infant is remote; or the product is not orally bioavailable in an infant.
Hale TW, Medications and Mother's Milk. Amarillo, TX: Hale Publishing L.P., 2006 p.34-35
Emergency Use Authorization (FDA/CDC)
No Emergency Use Authorization for Ibuprofen has been issued from the Food and Drug Administration under section 564 of the Federal Food, Drug and Cosmetic Act (FD&C Act) (21 U.S.C. 360bbb-3), amended by the Project Bioshield Act of 2004 (Public Law 108-276).
DHHS/FDA; Emergency Preparedness and Response-Counterterrorism and Emerging Threats (12/01/2011)
6. Current available formulations/shelf life
Formulation
-
Oral Capsules, liquid filled 200 mg ibuprofen*
-
Oral Suspension 40 mg/mL ibuprofen*
-
Oral Suspension 100 mg/5mL ibuprofen*
-
Oral Tablets 200 mg ibuprofen*
-
Oral Tablets 400 mg ibuprofen*
-
Oral Tablets 600 mg ibuprofen*
-
Oral Tablets 800 mg ibuprofen*
-
Oral Tablets, chewable 50 mg ibuprofen*
-
Oral Tablets, chewable 100 mg ibuprofen*
-
Oral Tablets, film-coated 100 mg ibuprofen*
-
Oral Tablets, film-coated 200 mg ibuprofen*
-
Oral Tablets, film-coated 400 mg ibuprofen*
-
Oral Tablets, film-coated 600 mg ibuprofen*
-
Oral Tablets, film-coated 800 mg ibuprofen*
-
Parenteral injection concentrate for iv use 100 mg/mL
-
Parenteral injection concentrate for iv use only 10 mg/mL (of ibuprofen)
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
Storage
-
Oral preparations containing ibuprofen should be stored in well-closed, light-resistant containers at 20-25°C.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Ibuprofen injection concentrate should be stored at 20-25°C. The product contains no preservatives.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Ibuprofen lysine injection should be stored at 20-25°C; the injection should be stored in the manufacturer's carton until time of use and should be protected from light. The product contains no preservatives and is intended for single use only; any unused portions should be discarded.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
7. Current off label utilization and dosing
— including children-, pregnancy-, geriatric-, and obesity-related dataAdult
-
Drugs to prevent inflammation and pulmonary edema as a result of chemically induced lung injury are needed. Several drugs that have been approved by the FDA for other indications hold promise for treating chemically induced pulmonary edema. These include β2-agonists, dopamine, insulin, allopurinol, and non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen. Inhaled and systemic forms of β2-agonists used in the treatment of asthma have been effective in reducing pulmonary edema in animal models but require further study.
DHHS/NIH; National Institute of Allergy and Infectious Diseases: Medical Countermeasures Against Chemical Threats-Respiratory Tract (NIH/NIAID)
8. Route of Administration/Monitoring
The lowest possible effective dosage and shortest duration of therapy consistent with treatment goals of the patient should be employed. Dosage of ibuprofen must be carefully adjusted according to individual requirements and response, using the lowest possible effective dosage. Patients receiving ibuprofen for self-medication should be advised to use the lowest effective dosage and not to exceed the recommended dosage or duration of therapy.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
9. Adverse effects
WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
-
Cardiovascular Risk
Non-steroidal anti-inflammatory drugs (NSAIDs) may increase the risk of serious cardiovascular (CV) thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk.
-
Gastrointestinal Risk
NSAIDs increase the risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events
Product label CALDOLOR (ibuprofen) injection [Cumberland Pharmaceuticals Inc.] Last revised: June 2009 [DailyMed]
-
Cardiovascular Effects:
Peripheral edema and fluid retention have been reported during ibuprofen therapy. Congestive heart failure has occurred in patients with marginal cardiac function. Increased blood pressure, hypotension, cerebrovascular accident, and palpitations also have been reported. Although a causal relationship has not been established, arrhythmias, including sinus tachycardia or bradycardia, have been reported during therapy with the drug.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
GI Effects:
The most frequent adverse effects of ibuprofen involve the GI tract and have included dyspepsia, heartburn, nausea, vomiting, anorexia, diarrhea, constipation, stomatitis, flatulence, bloating, epigastric pain, and abdominal pain. Peptic ulcer and GI bleeding (including evidence of occult blood in stools), sometimes severe, have also been reported. Although a causal relationship has not been established, a few cases of GI ulceration with perforation and bleeding resulting in death have occurred.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Nervous System Effects:
Adverse CNS effects of ibuprofen include dizziness, headache, and nervousness. Fatigue, drowsiness, malaise, lightheadedness, anxiety, confusion, mental depression, and emotional lability have also been reported. Although a causal relationship has not been established, paresthesia, hallucinations, dream abnormalities, and pseudotumor cerebri also have been reported. Aseptic meningitis with fever and coma has occurred rarely in patients receiving ibuprofen, and has recurred upon rechallenge with the drug.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Otic and Ocular Effects:
Patients receiving ibuprofen have experienced tinnitus. Decreased hearing and amblyopia (blurred and/or decreased visual acuity, scotomata and/or changes in color vision) have also been reported. Vision generally has gradually improved when the drug was discontinued in patients with visual disturbances. Although a causal relationship has not been established, conjunctivitis, diplopia, optic neuritis, and cataracts have also been reported in patients receiving the drug. Ibuprofen should be discontinued and an ophthalmologic examination performed in patients who experience visual disturbances during therapy with the drug.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Hepatic Effects:
Severe hepatic reactions (sometimes fatal) including jaundice and hepatitis have occurred rarely during ibuprofen therapy. A transitory rise in serum AST (SGOT), ALT (SGPT), and serum alkaline phosphatase has occurred in a few patients during ibuprofen therapy.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Dermatologic Effects:
Urticarial, vesiculobullous, and erythematous macular rashes, erythema multiforme, exfoliative dermatitis, toxic epidermal necrolysis (Lyell's syndrome), and photosensitivity reactions have occurred occasionally during ibuprofen therapy. Pruritus without evidence of a rash has occurred in a few patients. Stevens-Johnson syndrome, flushes, alopecia, rectal itching, and acne have also been reported.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Hematologic Effects:
Adverse hematologic effects of ibuprofen include neutropenia, agranulocytosis, aplastic anemia, hemolytic anemia (with or without positive direct antiglobulin test results), and thrombocytopenia (with or without purpura). Slight, dose-dependent reductions in serum hemoglobin concentrations and hematocrit have occurred in patients receiving ibuprofen dosages of 1.2-3.2 g daily, and the total decrease in hemoglobin may exceed 1 g in patients receiving 3.2 g or more of the drug. ... Although a causal relationship has not been established, bleeding episodes (e.g., epistaxis, menorrhagia, occult blood in the stool) have been reported during therapy with the drug. Ibuprofen can inhibit platelet aggregation and may prolong bleeding time.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Renal Effects:
Acute renal failure has been reported in patients receiving ibuprofen and may be accompanied by acute tubular necrosis. ... In addition, acute interstitial nephritis accompanied by hematuria, proteinuria, and occasionally nephrotic syndrome has occurred. Recurrence of nephrotic syndrome has occurred in at least one patient during ibuprofen therapy.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
Other Adverse Effects:
Hypersensitivity reactions manifested as a syndrome of abdominal pain, fever, chills, nausea, and vomiting have occasionally occurred during ibuprofen therapy. Anaphylaxis, anaphylactoid reactions, and bronchospasm have also occurred. Although a causal relationship has not been established, serum sickness, lupus erythematosus syndrome, Henoch-Schönlein vasculitis, and angioedema have also been reported during therapy with the drug.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
10. Contraindication(s)
-
Ibuprofen is contraindicated in patients with known hypersensitivity to the drug. NSAIAs generally are contraindicated in patients in whom asthma, urticaria, or other sensitivity reactions are precipitated by aspirin or other NSAIAs, since there is potential for cross-sensitivity between NSAIAs and aspirin, and severe, often fatal, anaphylactic reactions may occur in such patients.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
-
NSAIAs are contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery.
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
11. Clinical studies in progress
— including relevant ones and any others highlighting possible adverse effects and other effects/issues- No data available at this time.
12. Non-clinical studies in progress
— including relevant ones and any others highlighting possible adverse effects and other effects/issues- No data available at this time.
13. Needed studies for Chemical Defense clinical indication
— including pharmacokinetics, safety, efficacy, pregnancy, breastfeeding, and review panel recommendations- No data available at this time.
14. Needed studies for non Chemical Defense clinical indications
— including review panel recommendations- No data available at this time.
15. Study-related ethical concerns
— including review panel recommendations- No data available at this time.
16. Global regulatory status
U.S.
-
Ibuprofen injection
Ibuprofen is indicated in adults for the management of mild to moderate pain and the management of moderate to severe pain as an adjunct to opioid analgesics.
Product label CALDOLOR (ibuprofen) injection [Cumberland Pharmaceuticals Inc.] Last revised: June 2009 [DailyMed]
17. Other potentially useful information
-
Octanol/Water Partition Coefficient:
log Kow= 3.97
-
Solubility in water, 21 mg/l at 25 deg C
HSDB. Ibuprofen
18. Publications
Aranda JV, Varvarigou A, Beharry K, Bansal R, Bardin C, Modanlou H, Papageorgiou A, Chemtob S; Pharmacokinetics and protein binding of intravenous ibuprofen in the premature newborn infant. Acta Paediatr. 1997 Mar; 86 (3): 289-93.[PubMed Citation]
Borak J, Diller WF; Phosgene exposure: mechanisms of injury and treatment strategies. J Occup Environ Med 2001; 43 (2): 110-9. [PubMed Citation]
Briggs GG, Freeman RK, Yaffe SJ, eds.: Drugs in Pregnancy and Lactation, Ninth Edition. Lippincott Williams & Wilkins, Philadelphia, PA 2008 p.714-716
Cowan FM, Smith WJ et al.; Sulfur Mustard- And Phosgene- Increased IL-8 In Human Small Airway Cell Cultures: Implications For Medical Countermeasures Against Inhalation Toxicity. Proceedings of the U.S. Army Medical Defense Bioscience Review. (2005). [PubMed Citation]
DHHS/FDA; Emergency Preparedness and Response-Counterterrorism and Emerging Threats (12/01/2011)
DHHS/NIH; National Institute of Allergy and Infectious Diseases: Medical Countermeasures Against Chemical Threats-Respiratory Tract (NIH/NIAID)
Hale TW, Medications and Mother's Milk. Amarillo, TX: Hale Publishing L.P., 2006 p.455-456
HSDB. Ibuprofen
Kennedy TP et al; Ibuprofen prevents oxidant lung injury and in vitro lipid peroxidation by chelating iron. J Clin Invest. 1990; 86 (5): 1565-73 (1990) [PubMed Citation]
McEvoy GK, ed. Drug Information 2012. Bethesda, MD: American Society of Health-System Pharmacists, 2012 p.2121-2128
Product label CALDOLOR (ibuprofen) injection [Cumberland Pharmaceuticals Inc.] Last revised: June 2009 [DailyMed]
Rudy AC, Knight PM, Brater DC, Hall SD; Enantioselective disposition of ibuprofen in elderly persons with and without renalimpairment. J Pharmacol Exp Ther. 1995 Apr; 273 (1):88-93. [PubMed Citation]
Sciuto AM, Hurt HH; Therapeutic treatments of phosgene-induced lung injury. Inhalation Toxicology 2004; 16 (8): 565-80. [PubMed Citation]
Sciuto AM et al; Efficacy of ibuprofen and pentoxifylline in the treatment of phosgene-induced acute lung injury. J Appl Toxicol 1996; 16 (5): 381-4 (1996) [PubMed Citation]
19. Web sites
NIH CounterACT Program (HHS/NIH)
NIH RePORTER (HHS/NIH)
ClinicalTrials.gov (HHS/NIH)
PubMed (HHS/NIH)
DailyMed (HHS/NIH)
Record last updated 1/2/2013
