You are here: Home > Medical Countermeasures Database > Obidoxime
Obidoxime - Medical Countermeasures Database
- Name of Chemical Defense therapeutic agent/device
- Chemical Defense therapeutic area
- Evidence-based medicine for Chemical Defense
- Pharmacokinetic and toxicokinetics data
- Indication/dosing
- Formulation/shelf life
- Off-label use & dosing
- Route of administrating/monitoring
- Adverse effects
- Contraindications
- Clinical studies in progress
- Non-clinical studies in progress
- Needed studies for Chemical Defense
- Needed studies for non-Chemical Defense
- Study-related ethical concerns
- Global regulatory status
- Other potentially useful information
- Publications
- Web sites
1. Name of Chemical Defense therapeutic agent/device
Obidoxime
2. Chemical Defense therapeutic area(s)
— including key possible usesAntidote for organophosphorous nerve agent poisoning including chlorosarin, cyclosarin (GF), R-33 (VR), R-VX, sarin (GB), tabun (GA), VX, chlorosoman, soman (GD), and organophosphorous pesticides.
3. Evidence-based medicine for Chemical Defense
— including efficacy and safetyA. Summary
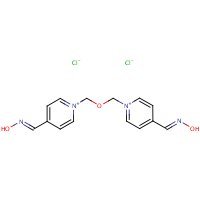
Structure
US NLM. ChemIDplus Lite. Obidoxime
Mechanism of action
-
Current treatment of organophosphorus poisoning, resulting in overstimulation and desensitization of muscarinic and nicotinic receptors by acetylcholine (ACh), consists of the administration of atropine and oxime reactivators. However, no versatile oxime reactivator has been developed yet and some mortality still remains after application of standard atropine treatment, probably due to its lack of antinicotinic action. In our study, we focused on the interesting non-acetylcholinesterase property of oximes, i.e. antinicotinic effect of reactivators. Two standard reactivators (HI-6, obidoxime) and two new compounds (K027 and K203) were chosen for in vitro (patch clamp) and in vivo (nerve-evoked muscle contraction) testings. Both examinations showed antinicotinic effects of the reactivators. In vitro inhibition of acetylcholine-evoked currents by obidoxime, HI-6 and K203 was equivalent while K027 was less potent. Similar order of potency was observed by the in vivo examinations. We thus confirm previous in vitro results, which describe antinicotinic effects of oxime reactivators, and furthermore, we show in vivo antagonism of oxime reactivators exerted by the inhibition of ACh effect on the nicotinic receptor in the neuromuscular junction. Taking together, the effects of tested oxime reactivators indicate an antagonism on both embryonic and adult form of the muscle nicotinic receptors.
Soukup O, Krůšek J, Kaniaková M, Kumar UK, Oz M, Jun D, Fusek J, Kuča K, Tobin G. Oxime reactivators and their in vivo and in vitro effects on nicotinic receptors. Physiol Res. 2011;60(4):679-86. [PubMed Citation]
-
Obidoxime, a well-known bis-pyridinium reactivator, is often the preferred antidote of organophosphorus poisoning caused by pesticides and tabun. It is also considered to be an allosteric modulator of muscarinic receptors, preferably M2 sub-type. This study compared the effect of obidoxime and atropine in vivo and in vitro on the cholinergic stimulation of the rat heart (M2) and the urinary bladder (M3). The results showed that obidoxime exerts anti-muscarinic effects, that may play an important role in the treatment of organophosphourus poisoning, and that the muscarinic receptor inhibition profile shows M2 receptor selectivity. This anti-muscarinic effect is much smaller that the effect of atropine and might be due to the allosteric inhibition of the receptors. The results also indicate that the acetylcholinesterase inhibition and the muscarinic receptor antagonism occur at different concentrations and dose levels.
Soukup O, Tobin G, Kumar UK, Jun D, Fusek J, Kuca K. Characterization of the anticholinergic properties of obidoxime; functional examinations of the rat atria and the urinary bladder. Toxicol Mech Methods. 2010 Sep;20(7):428-33. [PubMed Citation]
-
Organophosphorus poisoning manifests as a cholinergic syndrome due to an inhibition of acetylcholinesterase. It is treated symptomatically by anticholinergics and oxime reactivators are used as causal antidotes. Reactivators possess a complex mechanism of action and interact at various levels of the cholinergic transmission. The aim of this study was to investigate the effect of standard oxime reactivators (HI-6, obidoxime, trimedoxime, methoxime and pralidoxime) on the hemicholinium-3 sensitive carriers, which are involved in the high-affinity choline uptake (HACU) transport, a key regulatory step in the synthesis of acetylcholine. The activity of the carriers was estimated in vitro on hippocampal synaptosomes using the substrate (3H)-choline and the competitive inhibitor (3H)-hemicholinium-3. Furthermore, the effect of the reactivators on the fluidity of hippocampal membranes was assessed. All tested compounds, except methoxime, showed an acute inhibitory effect on the carriers, however, only at μM concentrations. Trimedoxime showed the highest potency to inhibit HACU among all tested compounds (I(max) 62%, IC(50)=3μM). All compounds, except HI-6, influenced also a membrane fluidity in the region of the hydrophilic heads of phospholipid bilayer, nevertheless, only methoxime was able to penetrate more deeply into the hydrocarbon core. We suggest that the direct interaction of oxime reactivators with the carrier protein (HI-6 and trimedoxime) and/or the changes in carrier conformation mediated by alterations in membrane fluidity (trimedoxime, obidoxime and pralidoxime) could occur here. The influence of reactivators on the carriers could be unfavorable in the case of their prolonged administration in vivo. From this point of view, the application of methoxime appears to be the best.
Soukup O, Kristofikova Z, Jun D, Tambor V, Ripova D, Kuca K. The interaction of standard oxime reactivators with hemicholinium-3 sensitive choline carriers. Toxicol Lett. 2012 Aug 3;212(3):315-9. [PubMed Citation]
-
There is an ongoing debate whether oximes can effectively counteract the effects of organophosphorus compounds (OP) on brain acetylcholinesterase (AChE) activity and whether there are differences in the kinetic properties of brain and erythrocyte AChE. In order to investigate the kinetics of AChE from different tissues and species the well established dynamically working in vitro model with real-time determination of membrane-bound AChE activity was adapted for use with brain AChE. The enzyme reactor, that was loaded with brain, erythrocyte or muscle AChE, was continuously perfused with substrate and chromogen while AChE activity was on-line analyzed in a flow-through detector. It was possible to determine the Michaelis-Menten constants of human erythrocyte, muscle and brain AChE which were almost identical. In addition, the inhibition kinetics of sarin and paraoxon as well as the reactivation kinetics of obidoxime and HI 6 were determined with human, swine and guinea pig brain and erythrocyte AChE. It was found that the inhibition and reactivation kinetics of brain and erythrocyte AChE were highly comparable in all tested species. These data support the view that AChE from different tissue has similar kinetic properties and that brain AChE is comparably susceptible toward reactivation by oximes.
Herkert NM, Freude G, Kunz U, Thiermann H, Worek F. Comparative kinetics of organophosphates and oximes with erythrocyte, muscle and brain acetylcholinesterase. Toxicol Lett. 2012 Mar 7;209(2):173-8. [PubMed Citation]
-
The purpose of this work was to evaluate the possible non-reactivating effects of toxogonin (1,1'[oxybis(methylene)]bis[4-[hydroxyimino) methyl]pyridinium]-dichloride), HI-6 (1-[[[(4-aminocarbonyl)pyridinio] methoxy]methyl]-2-[(hydroxyimino)methyl]pyridinium-dichloride) and HLö-7 (pyridinium, 1-[[[4-(aminocarbonyl)pyridino]methoxy] methyl]-2,4-bis-[(hydroxyimino)methyl]diiodide) on the release of acetylcholine from cholinergic nerves. The oximes have been tested in our rat bronchial smooth muscle model, with respect to the effects of oximes on the K+ (51 mM)-evoked release of [3H]acetylcholine in the presence and absence of soman (1.0 microM). Toxogonin (100 microM) had no effect on the K(+)-evoked release of [3H]acetylcholine in the presence or absence of soman (1.0 microM). Similar results were found for HI-6 (100 microM). In contrast, HLö-7 (100 microM) enhanced the K(+)-evoked release of [3H]acetylcholine in the absence of soman. In the presence of soman HLö-7 did not alter the release of [3H]acetylcholine induced by K+ stimulation. The potentiating effect of HLö-7 on the release of [3H]acetylcholine could be blocked by the L-, N- and P-Ca2+ channel blockers verapamil (0.1 and 1.0 microM), omega-conotoxin GVIA (1.0 microM) and omega-agatoxin IV-A (0.2 microM), respectively. Muscarinic receptor antagonists (atropine (10 microM), pirenzepine (M1) (1.0 microM) and methoctramine (M2) (1.0 microM) had no effects on the HLö-7 (100 microM)-enhanced release of [3H]acetylcholine. Protein kinase inhibitors (H-7 (20 microM), calphostin C (1.0 microM) and KN-62 (10 microM) inhibited the HLö-7 (100 microM)-enhanced K(+)-evoked release of [3H]acetylcholine. The results showed that only HLö-7 had a direct enhancing effect on the release of acetylcholine through activation or opening of Ca2+ channels and a subsequent protein phosphorylation in the nerve terminal.
Aas P. In vitro effects of toxogonin, HI-6 and HLö-7 on the release of [3H]acetylcholine from peripheral cholinergic nerves in rat airway smooth muscle. Eur J Pharmacol. 1996 Apr 22;301(1-3):59-66. [PubMed Citation]
Summary of clinical and non-clinical studies
Acute organophosphate (OP) toxicity is primarily caused by inhibition of cholinesterase (acetylcholinesterase [AChE] or butyrylcholinesterase [BChE], which leads to an accumulation of acetylcholine (ACh) or butyrylcholine (BCh) and subsequent impairment of body functions. Standard treatment of acute OP toxicity combines an antimuscarinic compound (e.g. atropine), occasionally an anticonvulsant (e.g. diazepam), and an AChE reactivator (e.g. obidoxime). The efficacy of obidoxime to reactivate AChE or BChE inhibited by OP pesticides or nerve agents has been tested in several studies.
In vitro studies demonstrated that obidoxime was most effective (reactivation efficacy of 96.8%) at reactivating human AChE inhibited by the OP pesticide paraoxon than other oximes (trimedoxime, pralidoxime, methoxime, and HI-6; ≤25% reactivation efficacy) (Jun et al., 2008). The reactivation efficacy of obidoxime also extended to human AChE inhibited by other OP pesticides, including leptophos-oxon and methamidophos, and to paraoxon-inhibited AChE from various species (human, Rhesus monkey, swine, rabbit, rat, and guinea pig) (Jun et al., 2010; Jun et al., 2011; Worek et al., 2011). However, obidoxime seems to be less effective at reactivating human BChE inhibited by OP pesticides (≤15% reactivation) (Jun et al., 2008; Jun et al., 2011). Obidoxime also failed to demonstrate a strong therapeutic efficacy against OP pesticide poisoning in a prospective clinical study (Balali-Mood and Shariat, 1998). Intravenous obidoxime or pralidoxime (8 mg/kg and 30 mg/kg loading doses, respectively) combined with atropine, or atropine alone, was administered to 63 OP pesticide-poisoned patients. A high mortality rate (6 of 12 patients, 50%) occurred in the obidoxime plus atropine group, whereas no mortality occurred in patients that received pralidoxime plus atropine (0 of 8 patients). AChE activity decreased over a 10-day period for the obidoxime plus atropine group, but increased for the pralidoxime plus atropine group. Although not statistically significant (r = 0.4747), AChE reactivation was only observed in the pralidoxime plus atropine group.
The efficacy of obidoxime as a cholinesterase reactivator appears to be nerve agent specific. Obidoxime was not as effective as HI-6 in reactivating soman- and sarin-inhibited AChE purified from human caudate nucleus and skeletal muscle, but it was more effective for tabun-inhibited enzyme (Puu et al., 1986). In reactivating soman-inhibited AChE from rat brain homogenate, obidoxime was ineffective; in contrast, it was the most effective reactivator against tabun-inhibited AChE compared to pralidoxime, trimedoxime, methoxime, and HI-6 (Kuca et al., 2007). This finding is parallel to another in vitro study that observed satisfactory obidoxime reactivation of tabun-inhibited AChE from rat brain homogenate (Kuca et al., 2006a). Another study also demonstrated the effectiveness of obidoxime in reactivating human AChE inhibited by tabun as well as by phosphonoamidate analogues of tabun (Worek et al., 2007). After incubation of tabun-inhibited AChE from humans with obidoxime or with other oximes including TMB-4, MMB-4, HI-6, or HLö7 (1mM, 37°C), obidoxime was the second most potent reactivator. The reactivating potency of obidoxime was inversely proportional to the chain length of the tabun analogues. The reactivation potency of obidoxime towards cyclosarin-inhibited AChE was exceeded by the oximes HI-6, BI-6, and HS-6, and was too low to calculate, in in vitro experiments using rat brain homogenate (Bartosova et al., 2005). Although in vivo, obidoxime reduced the acute toxicity of cyclosarin 1.5-fold in mice and almost 5-fold in rats, the other oximes tested (HI-6, BI-6, and HS-6) were more effective. Obidoxime was unable to sufficiently reactivate cyclosarin-inhibited AChE from rat brain homogenate; it was, however, able to reactivate sarin-inhibited AChE, although at a concentration that is toxic for humans (Kuca et al., 2005). In reactivating VX-inhibited AChE obtained from rat brain homogenate, the reactivation potency of obidoxime was less than that of oximes TO205, TO046, HI-6, K027, and HS-6 (Kuca and Kassa, 2004). The reactivation efficacy of obidoxime on VX-inhibited AChE from rat brain homogenate was also surpassed by HI-6, HLö7, and BI-6, except in the case of tabun-inhibited AChE (Kuca et al., 2006b). Another study found obidoxime to be effective at significantly reactivating VX- and Russian VX-inhibited cholinesterases from rat brain homogenate, but only at concentrations that exceed the recommended in vivo doses (Kuca et al., 2006c). The use of obidoxime in treating acute OP toxicity may increase the risk of bleeding, and at high doses, may induce hepatotoxicity and liver dysfunction (Balali-Mood and Shariat, 1998; Jun et al., 2006).
B. Link to clinical studies
Adult
-
1 The effectiveness of oxime therapy in organophosphate poisoning is still a matter of debate. It appears, however, that the often cited ineffectiveness of oximes may be due to inappropriate dosing. By virtue of in vitro findings and theoretical considerations we concluded in the preceding paper that oximes should preferably be administered by continuous infusion following an initial bolus dose for as long as reactivation of inhibited acetylcholinesterase (AChE) can be expected. This conclusion has called for a clinical trial to evaluate such oxime therapy on the basis of objective parameters. 2 Before transfer to the intensive care unit (ICU), 5 patients received primary care by an emergency physician. In the ICU, atropine sulphate was administered i.v. upon demand according to the endpoints: no bronchorrhoea, dry mucous membranes, no axillary sweating, heart rate of about 100/min. Obidoxime (Toxogonin) was given as an i.v. bolus (250 mg) followed by continuous infusion of 750 mg/24 h. 3 Intoxication and therapy were monitored by determining erythrocyte AChE (eryAChE) activity, reactivatability of the patient's eryAChE ex vivo, plasma cholinesterase activity, the presence of AChE inhibiting compounds, as well as the concentrations of obidoxime and atropine in plasma. 4 Obidoxime was effective in life-threatening parathion poisoning, in particular when the dose absorbed was comparably low. In mega-dose poisoning, net reactivation was not achieved until several days after ingestion, when the concentration of active poison in plasma had declined. Reactivatability in vivo lasted for a longer period than expected from in vitro experiments. 5 Obidoxime was quite ineffective in oxydemetonmethyl poisoning, when the time elapsed between ingestion and oxime therapy was longer than 1 day. When obidoxime was administered shortly after ingestion (1 h) reactivation was nearly complete. 6 Obidoxime levels of 10-20 microM were achieved by our regimen, and atropine could rapidly be reduced to approx. 20 microM, as attained by continuous infusion of 1 mg atropine sulphate/h. Maintenance of the desired plasma levels was not critical even when renal function deteriorated. 7 Signs of transiently impaired liver function were observed in patients who showed transient multiorgan failure. In the present stage of knowledge, we feel it advisable to keep the plasma concentration of obidoxime at 10-20 microM, although the full reactivating potential of obidoxime will not then be exploited. Still, the reactivation rate, with an apparent half-time of some 3 min, is twice that estimated for a tenfold higher pralidoxime concentration. (Class IV)
Thiermann H, Mast U, Klimmek R, Eyer P, Hibler A, Pfab R, Felgenhauer N, Zilker T. Cholinesterase status, pharmacokinetics and laboratory findings during obidoxime therapy in organophosphate poisoned patients. Hum Exp Toxicol. 1997 Aug;16(8):473-80. [PubMed Citation]
-
Thirty-four adult patients with severe organophosphorus compounds (OP) poisoning requiring artificial ventilation were enrolled in a clinical study and received atropine and obidoxime (250 mg i.v., followed by 750 mg/24 h) as antidotal treatment. Here, we re-analyzed the cholinesterase status (red blood cell acetylcholinesterase (RBC-AChE) activity, reactivatability of RBC-AChE, and plasma butyrylcholinesterase (Pl-BChE) activity) in relation to the neuromuscular transmission (NMT) data. When RBC-AChE activity ranged between 100% and 30% NMT was unimpaired after tetanic stimulation with frequencies up to 50 Hz. A further decrease in RBC-AChE activity was accompanied by a marked disturbance of NMT, being strongly impaired at AChE activities <5% of normal. Higher stimulation frequencies (>30 Hz) facilitated the discrimination of the types of impairment. The neuromuscular transmission was the best quantified by using the ratio of the ninth to the first amplitude, while the standard method was less discriminative. At RBC-AChE levels higher than 40% of normal weaning from the ventilator may be considered. Completely aged RBC-AChE as indicated by loss of reactivatability loses its guidance function. Then, steadily increasing Pl-BChE activity suggests lack of circulating poison. One-week later, neuromuscular transmission may be largely normal and patients could be weaned from the respirator if other complications are not withstanding. (Class III)
Thiermann H, Zilker T, Eyer F, Felgenhauer N, Eyer P, Worek F. Monitoring of neuromuscular transmission in organophosphate pesticide-poisoned patients. Toxicol Lett. 2009 Dec 15;191(2-3):297-304. [PubMed Citation]
-
A 50-year-old man swallowed 200 ml of an insecticide containing the organophosphates dimethoate and phenitrotion in an attempted suicide. On admission, signs of a cholinergic syndrome were observed: miosis, rhinorrhoea, and fasciculations. This was followed by bradycardia with hypotension and vomiting. The patient was treated with the antidotes atropine and obidoxime. Decreasing consciousness necessitated intubation, mechanical ventilation and other supportive measures. Although the serum concentrations of both organophosphate compounds rapidly decreased, the activity of cholinesterase showed a prolonged inhibition. The clinical course was complicated by hypotension, acute respiratory distress syndrome, nosocomial pneumonia, and an epileptic seizure. A period with muscle weakness and a persisting depressive disorder then followed. This case is characteristic for acute intoxications with irreversible acetylcholinesterase inhibitors, such as organophosphate compounds. The treatment of these potentially severe intoxications includes rapid decontamination and the administration of high doses of atropine followed by obidoxime. Mechanical ventilation and circulatory support are also indicated. (Class IV)
Vos EM, Hens JJ, Lau HS, Boon ES, Bartelink AK. Poisoning with organophosphate compounds. Ned Tijdschr Geneeskd. 2002 Jan 5;146(1):34-7. {PubMed Citation]
-
OBJECTIVE: The effects of obidoxime in the treatment of organophosphate poisoning were assessed by comparing the clinical course with its effects on laboratory parameters relevant to poisoning. In this article we report clinical findings and activity of cholinesterase in plasma and acetylcholinesterase (AChE) in red blood cells. In a linked paper we describe changes in neuromuscular transmission and atropine concentrations in the same patient cohort. METHODS: We studied 34 atropinized patients with severe parathion, oxydemeton methyl, and dimethoate self-poisoning who were treated with obidoxime in a standard protocol. We measured the AChE activity in blood and related it to clinical features of organophosphate poisoning. RESULTS: Patients poisoned with parathion responded promptly to obidoxime (250 mg bolus followed by continuous infusion at 750 mg/day up to 1 week) with improvement of neuromuscular transmission and increased AChE activity. The effects were only transient in cases with the other poisons. Death (7/34) occurred late and was mostly due to complications rather than due to ongoing cholinergic crisis. CONCLUSIONS: Obidoxime appeared safe and reactivated AChE in parathion poisoning. (Class IV)
Eyer F, Worek F, Eyer P, Felgenhauer N, Haberkorn M, Zilker T, Thiermann H. Obidoxime in acute organophosphate poisoning: 1 - clinical effectiveness. Clin Toxicol (Phila). 2009 Sep;47(8):798-806. [PubMed Citation]
-
Out of 859 consecutive cases treated for exposure to organophosphate (PO) insecticides, 53 were included in the study. Criteria for inclusion were severe OP poisoning necessitating artificial ventilation, intensive care monitoring and treatment according to a standard protocol. The protocol was based on relatively high doses of obidoxime, relatively low doses of atropine and overriding with a pacemaker in cases of ventricular arrhythmias and prolonged Q-T interval. Seven patients died during hospitalization. Thirty-two patients (60%) had major central nervous system (CNS) involvement. Five (9.4%) presented severe psychiatric sequelae. Twenty-two patients (41.5%) presented cardiac arrhythmias. Five (9.4%) had liver dysfunction. High frequency of cardiac arrhythmias was observed in patients who received high cumulative doses of atropine and obidoxime; impairment of liver functions was significantly higher in patients who received high cumulative doses of obidoxime. We conclude that each drug should be titrated separately: atropine dosage should be adjusted to the severity of tracheobronchial secretions and bronchospasm, while full doses of obidoxime are justified for the period before "aging" sets in. (Class III)
Finkelstein Y, Kushnir A, Raikhlin-Eisenkraft B, Taitelman U. Antidotal therapy of severe acute organophosphate poisoning: a multihospital study. Neurotoxicol Teratol. 1989 Nov-Dec;11(6):593-6. [PubMed Citation]
-
Organophosphate (OP) compounds have been used as pesticides and in chemical warfare (nerve agents). Two nerve agents, tabun and sarine, were used by the Iraqi army against Iranian troops and innocent people. Hundreds of the exposed combatants died in the field. Atropine sulphate has been used successfully in large doses to counteract the muscarinic effects of OP poisoning. The effects of oximes in human OP poisoning have not been well studied. Our aim was to study the effects of obidoxime and pralidoxime in OP pesticide poisoning. The patients were divided into three groups: atropine (A), obidoxime + atropine (OA) and pralidoxime + atropine (PA). Sixty-three patients (33 males, 30 females) with a mean age of 25 years were studied in different groups (43 A, 22 OA and 8 PA). There were no statistical significant differences in major clinical findings and acetylcholinesterase (AChE) activity on admission between the groups. Significant changes were observed during the treatment. Notwithstanding the severity of intoxication--particularly respiratory complications were more observed in the OA and PA groups--there were no fatalities in the PA group, whereas 4 (9%) and 6 (50%) patients in the A and OA groups died, respectively. AChE reactivation was only observed in the PA group, although it was not statistically significant (r = 0.4747). There was a good relationship between the AChE reactivation and outcome of the patients. High doses of obidoxime (8 mg/kg followed by 2 mg/kg/h) were found to be hepatotoxic and should be avoided. High doses of pralidoxime (30 mg/kg followed by 8 mg/kg/h) did not induce serious side effects and may be effective in some OP pesticides poisoning. (Class III)
Balali-Mood M, Shariat M. Treatment of organophosphate poisoning. Experience of nerve agents and acute pesticide poisoning on the effects of oximes. J Physiol Paris 1998 Oct-Dec;92(5-6):375-8 [PubMed Citation]
Pediatric studies
-
OBJECTIVE: (1) Retrospective evaluation of the clinical course of carbamate poisoning and the effect of oxime therapy in children. (2) In vitro study of the effect of oximes on the reactivation of carbamylated cholinesterase. DESIGN: (1) Clinical survey: The records of 26 children intoxicated with carbamates were examined retrospectively. The poisoning agents in all cases were positively identified as methomyl or aldicarb by gas chromatography-mass spectrometry. (2) Laboratory study: The direct effect of obidoxime and of pralidoxime on acetylcholinesterase activity in vitro was investigated in normal human packed red blood cells pretreated with an organophosphate (paraoxon) or a carbamate (aldicarb or methomyl). CLINICAL SETTING: Pediatric intensive care unit of a teaching hospital. PATIENTS: Twenty-six infants and young children (aged 1 to 8 years) admitted to the pediatric intensive care unit with severe carbamate intoxication. INTERVENTIONS: All cases had been treated with repeated doses of atropine sulfate (0.05 mg/kg) administered every 5 to 10 minutes until muscarinic symptoms disappeared. Obidoxime chloride (Toxogonin, 6 mg/kg) was administered on admission, and again after 4 to 5 hours. RESULTS: Predominant symptoms were related to central nervous system and nicotinic effects. All the patients showed marked improvement within several hours and recovered completely within 24 hours. None of the children deteriorated and none showed exacerbation of cholinergic symptoms after obidoxime treatment. In vitro, oximes reactivated acetylcholinesterase inhibited with paraoxon, whereas no significant effect of oximes on carbamylated enzyme activity was observed. CONCLUSIONS: Based on the recovery of all cases, as compared with other reports of carbamate poisoning treated with atropine alone, it is concluded that, in the case of aldicarb or methomyl poisoning, oxime therapy apparently does not contribute to the recovery of poisoned patients. In cases of poisoning by an unknown pesticide or of mixed poisoning, oxime therapy can prove beneficial because no negative effects of the therapy can be discerned. (Class III)
Lifshitz M, Rotenberg M, Sofer S, Tamiri T, Shahak E, Almog S. Carbamate poisoning and oxime treatment in children: a clinical and laboratory study. Pediatrics. 1994 Apr;93(4):652-5. [PubMed Citation]
-
A previously healthy 2-y-old boy was admitted to the hospital 30 min after the ingestion of 10 ml of demeton-S-methyl (META-SYSTOX). Treatment consisted of gastric decontamination, atropine, reactivator (obidoxime) and supportive therapy. Atropine was given to control the muscarinic features. Assisted ventilation was required for 6 h; however, this treatment was able to be discontinued following the second injection of obidoxime 11.5 h after the ingestion. Excess salivation and slight bradycardia were easily controlled with small doses of atropine for 5 d following admission to Ullevaal Hospital. Further course was uneventful, and the patient was discharged on the 8th d without any sequelae. Plasma cholinesterase levels were initially low (<400 U/l), but returned to reference values upon discharge. In this case, adequate supportive therapy and the rapid administration of both atropine and obidoxime were clearly associated with a favorable outcomes. (Class IV)
Rolfsjord LB, Fjaerli HO, Meidel N, Stromme JH, Kowalczyk M, Jacobsen D. Severe organophosphate (demeton-S-methyl) poisoning in a two-year-old child. Vet Hum Toxicol. 1998 Aug;40(4):222-4. [PubMed Citation]
-
INTRODUCTION: Exposure to organophosphate and carbamate insecticides inhibits cholinesterase activity and interferes with synaptic transmission both centrally and peripherally at muscarinic receptors and nicotinic receptors. The study reported the usefulness of plasma cholinesterase ChE activity assays for diagnosis and the management of organophosphate and carbamate toxicity in children. METHODS: A retrospective study was conducted on children with organophosphate and carbamate poisoning. Forty-seven patients were included. The diagnosis was confirmed by measuring plasma cholinesterase levels. Atropine was given intravenous (0.02 mg/kg) and repeated until secretions were controlled. Obidoxime chloride was administered as 4-8 mg/kg/dose for children with organophosphate poisoning and to those in whom the ingested material was unidentified on admission. DISCUSSION: Most of the patients showed marked reactivation in plasma ChE within several hours and recovered completely within 24 h of admission. Complications were observed in 17 patients (36%). Mechanical ventilatory support was required in six patients. The duration intensive care stay was 3 +/- 2.4 days. CONCLUSION: Low plasma ChE levels support the diagnosis of insecticides poisoning, but no significant association is present between the severity of poisoning and plasma ChE levels. Atropine should be used as soon as possible to counteract the muscarinic effects. Appropriate management and early recognition of the complications may decrease the mortality rate. (Class III)
El-Naggar Ael-R, Abdalla MS, El-Sebaey AS, Badawy SM. Clinical findings and cholinesterase levels in children of organophosphates and carbamates poisoning. Eur J Pediatr. 2009 Aug;168(8):951-6. Epub 2008 Nov 8. [PubMed Citation]
Clinical reviews
-
This paper reviews the mechanisms of interaction of organophosphorus compounds with cholinesterases and clinical signs of acute poisoning. Further, we describe the current understanding of the mechanisms of action of pyridinium oximes pralidoxime (PAM-2), trimedoxime (TMB-4), obidoxime (LüH-6, Toxogonin), HI-6 and HLö-7 which are used as cholinesterase reactivators in the treatment of poisoning with organophosphorus compounds. We also review the most important literature data related to the efficacy of these oximes in the treatment of poisoning with warfare nerve agents soman, sarin, tabun, VX and cyclosarin and organophosphorus insecticides. Finally, we discuss the criteria for selection of oximes intended for further development as antidotes in poisoning with organophosphorus compounds and auto-injectors for their application in urgent situations (Class IV).
Jokanović M, Stojiljković MP. Current understanding of the application of pyridinium oximes as cholinesterase reactivators in treatment of organophosphate poisoning. Eur J Pharmacol. 2006 Dec 28;553(1-3):10-7. [PubMed Citation]
-
There are important differences between on-target military attacks against relatively well protected Armed Forces and nerve agent attacks initiated by terrorists against a civilian population. In contrast to military personnel, civilians are unlikely to be pre-treated with pyridostigmine and protected by personal protective equipment. Furthermore, the time after exposure when specific therapy can first be administered to civilians is likely to be delayed. Even conservative estimates suggest a delay between exposure and the first administration of atropine/oxime of at least 30 minutes. The organophosphorus nerve agents are related chemically to organophosphorus insecticides and have a similar mechanism of toxicity, but a much higher mammalian acute toxicity, particularly via the dermal route. Nerve agents phosphonylate a serine hydroxyl group in the active site of the enzyme, acetylcholinesterase (AChE), which results in accumulation of acetylcholine and, in turn, causes enhancement and prolongation of cholinergic effects and depolarisation blockade. The rate of spontaneous reactivation of AChE is variable, which partly accounts for differences in acute toxicity between the nerve agents. With soman in particular, an additional reaction occurs known as 'aging'. This consists of monodealkylation of the dialkylphosphonyl enzyme, which is then resistant to spontaneous hydrolysis and reactivation by oximes. Monodealkylation occurs to some extent with all dialkylphosphonylated AChE complexes; however, in general, is only of clinical importance in relation to the treatment of soman poisoning, where it is a very serious problem. With soman, aging occurs so fast that no clinically relevant spontaneous reactivation of AChE occurs before aging has taken place. Hence, recovery of function depends on resynthesis of AChE. As a result, it is important that an oxime is administered as soon after soman exposure as possible so that some reactivation of AChE occurs before all the enzyme becomes aged. Even though aging occurs more slowly and reactivation occurs relatively rapidly in the case of nerve agents other than soman, early oxime administration is still clinically important in patients poisoned with these agents. Experimental studies on the treatment of nerve agent poisoning have to be interpreted with caution. Some studies have used prophylactic protocols, whereas the drugs concerned (atropine, oxime, diazepam) would only be given to a civilian population after exposure. The experimental use of pyridostigmine before nerve agent exposure, although rational, is not of relevance in the civilian context. With the possible exception of the treatment of cyclosarin (GF) and soman poisoning, when HI-6 might be preferred, a review of available experimental evidence suggests that there are no clinically important differences between pralidoxime, obidoxime and HI-6 in the treatment of nerve agent poisoning, if studies employing pre-treatment with pyridostigmine are excluded (Class IV).
Marrs TC, Rice P, Vale JA. The role of oximes in the treatment of nerve agent poisoning in civilian casualties. Toxicol Rev. 2006;25(4): 297-323. [PubMed Citation]
-
The increasing threat of nerve agent use for terrorist purposes against civilian and military population calls for effective therapeutic preparedness. At present, administration of atropine and an oxime are recommended, although effectiveness of this treatment is not proved in clinical trials. Here, monitoring of intoxications with organophosphorus (OP) pesticides may be of help, as their actions are closely related to those of nerve agents and intoxication and therapy follow the same principles. To this end, the clinical course of poisoning and the effectiveness of antidotal therapy were investigated in patients requiring artificial ventilation being treated with atropine and obidoxime. However, poisoning with OP pesticides shows extremely heterogeneous pictures of cholinergic crisis frequently associated with clinical complications. To achieve valuable information for the therapy of nerve agent poisoning, cases resembling situations in nerve agent poisoning had to be extracted: (a) intoxication with OPs forming reactivatable OP-AChE-complexes with short persistence of the OP in the body resembling inhalational sarin intoxication; (b) intoxication with OPs resulting rapidly in an aged OP-AChE-complex resembling inhalational soman intoxication; (c) intoxications with OPs forming a reactivatable AChE-OP complex with prolonged persistence of the OP in the body resembling percutaneous VX intoxication. From these cases it was concluded that sufficient reactivation of nerve agent inhibited non-aged AChE should be possible, if the poison load was not too high and the effective oximes were administered early and with an appropriate duration. When RBC-AChE activity was higher than some 30%, neuromuscular transmission was relatively normal. Relatively low atropine doses (several milligrams) should be sufficient to cope with muscarinic symptoms during oxime therapy (Class IV).
Thiermann H, Szinicz L, Eyer P, Felgenhauer N, Zilker T, Worek F. Lessons to be learnt from organophosphorus pesticide poisoning for the treatment of nerve agent poisoning. Toxicology. 2007 Apr 20;233(1-3):145-54. [PubMed Citation]
-
The use of organophosphorus pesticides results in toxicity risk to non-target organisms. Organophosphorus compounds share a common mode of action, exerting their toxic effects primarily via acetylcholinesterase (AChE) inhibition. Consequently, acetylcholine accumulates in the synaptic clefts of muscles and nerves, leading to overstimulation of cholinergic receptors. Acute cholinergic crisis immediately follows exposure to organophosphate and includes signs and symptoms resulting from hyperstimulation of central and peripheral muscarinic and nicotinic receptors. The current view of the treatment of organophosphate poisoning includes three strategies, i.e. the use of an anticholinergic drug (e.g., atropine), cholinesterase-reactivating agents (e.g., oximes) and anticonvulsant drugs (e.g., benzodiazepines). Oximes, as a part of antidotal therapy, ensure the recovery of phosphylated enzymes via a process denoted as reactivation of inhibited AChE. However, both experimental results and clinical findings have demonstrated that different oximes are not equally effective against poisonings caused by structurally different organophosphorus compounds. Therefore, antidotal characteristics of conventionally used oximes can be evaluated regarding how close the certain substance is to the theoretical concept of the universal oxime. Pralidoxime (PAM-2), trimedoxime (TMB-4), obidoxime (LüH-6), HI-6 and HLö-7 have all been demonstrated to be very effective in experimental poisonings with sarin and VX. TMB-4 and LüH-6 may reactivate tabun-inhibited AChE, whereas HI-6 possesses the ability to reactivate the soman-inhibited enzyme. An oxime HLö-7 seems to be an efficient reactivator of AChE inhibited by any of the four organophosphorus warfare agents. According to the available literature, the oximes LüH-6 and TMB-4, although relatively toxic, are the most potent to induce reactivation of AChE inhibited by the majority of organophosphorus pesticides. Since there are no reports of controlled clinical trials on the use of TMB-4 in human organophosphate pesticide poisoning, LüH-6 may be a better option (Class IV).
Antonijevic B, Stojiljkovic MP. Unequal efficacy of pyridinium oximes in acute organophosphate poisoning. Clin Med Res. 2007 Mar;5(1):71-82. [PubMed Citation]
-
The cholinesterase-inhibiting organophosphorus compounds referred to as nerve agents (soman, sarin, tabun, GF agent, and VX) are particularly toxic and are considered to be among the most dangerous chemical warfare agents. Included in antidotal medical countermeasures are oximes to reactivate the inhibited cholinesterase. Much experimental work has been done to better understand the properties of the oxime antidotal candidates including the currently available pralidoxime and obidoxime, the H oximes HI-6 and Hlö-7, and methoxime. There is no single, broad-spectrum oxime suitablefor the antidotal treatment of poisoning with all organophosphorus agents. If more than one oxime is available, the choice depends primarily on the identity of the responsible organophosphorus compound. The H oximes appear to be very promising antidotes against nerve agents because they are able to protect experimental animals from toxic effects and improve survival of animals poisoned with supralethal doses. They appear more effective against nerve agent poisoning than the currently used oximes pralidoxime and obidoxime, especially in the case of soman poisoning. On the other hand, pralidoxime and especially obidoxime seem sufficiently effective to treat poisonings with organophosphorus insecticides that have relatively less toxicity than nerve agents (Class IV).
Kassa J. Review of oximes in the antidotal treatment of poisoning by organophosphorus nerve agents. J Toxicol Clin Toxicol. 2002;40(6):803-16. [PubMed Citation]
C. Link to non-clinical (e.g., animal) studies
Adult animal studies
-
The mechanism of intoxication with organophosphorus compounds, including highly toxic nerve agents and less toxic pesticides, is based on the formation of irreversibly inhibited acetylcholinesterase, which causes cumulation of neuromediator acetylcholine in synaptic clefts and subsequent overstimulation of cholinergic receptors, that is followed by a generalized cholinergic crisis. Nerve agent poisoning is conventionally treated using a combination of a cholinolytic (atropine mostly) to counteract the accumulation of acetylcholine and acetylcholinesterase reactivators (pralidoxime or obidoxime) to reactivate inhibited acetylcholinesterase. In this study of cyclosarin poisoning treatment, oximes of different chemical structures (obidoxime, HI-6, BI-6, and HS-6) were tested in vitro on rat brain acetylcholinesterase (enzyme source: rat brain homogenate), and afterwards, they were tested in vivo in equimolar doses, in mice and rats. The HI-6 oxime appeared to be the most effective oxime in vitro and in vivo.
Bartosova L, Kuca K, Jun D, Kunesova G. Bispyridinium oximes as antidotal treatment of cyclosarin poisoning-in vitro and in vivo testing. Int J Toxicol. 2005 Nov-Dec;24(6):399-402. [PubMed Citation]
-
The influence of the combination of oximes on the reactivating and therapeutic efficacy of antidotal treament of acute tabun poisoning was evaluated. The ability of two combinations of oximes (HI-6 + obidoxime and HI-6 + K203) to reactivate tabun-inhibited acetylcholinesterase and reduce acute toxicity of tabun was compared with the reactivating and therapeutic efficacy of antidotal treatment involving single oxime (HI-6, obidoxime, K203) using in vivo methods. Studies determining percentage of reactivation of tabun-inhibited blood and tissue acetylcholinesterase in poisoned rats showed that the reactivating efficacy of both combinations of oximes is higher than the reactivating efficacy of the most effective individual oxime in blood and diaphragm and comparable with the reactivating effects of the most effective individual oxime in brain. Moreover, both combinations of oximes were found to be slightly more efficacious in the reduction of acute lethal toxic effects in tabun-poisoned mice than the antidotal treatment involving individual oxime. A comparison of reactivating and therapeutic efficacy of individual oximes showed that the newly developed oxime K203 is slightly more effective than commonly used obidoxime and both of them are markedly more effective than the oxime HI-6. Based on the obtained data, we can conclude that the antidotal treatment involving chosen combinations of oximes brings beneficial effects for the potency of antidotal treatment to reactivate tabun-inhibited acetylcholinesterase in rats and to reduce acute toxicity of tabun in mice.
Kassa J, Karasova JZ, Pavlikova R, Misik J, Caisberger F, Bajgar J. The influence of combinations of oximes on the reactivating and therapeutic efficacy of antidotal treatment of tabun poisoning in rats and mice. J Appl Toxicol. 2010 Mar;30(2):120-4. [PubMed Citation]
-
The nerve agent VX is most likely to enter the body via liquid contamination of the skin. After percutaneous exposure, the slow uptake into the blood, and its slow elimination result in toxic levels in plasma for a period of several hours. Consequently, this has implications for the development of toxic signs and for treatment onset. In the present study, clinical signs, toxicokinetics and effects on respiration, electroencephalogram and heart rate were investigated in hairless guinea pigs after percutaneous exposure to 500 microg/kg VX. We found that full inhibition of AChE and partial inhibition of BuChE in blood were accompanied by the onset of clinical signs, reflected by a decline in respiratory minute volume, bronchoconstriction and a decrease in heart rate. Furthermore, we investigated the therapeutic efficacy of a single dose of atropine, obidoxime and diazepam, administered at appearance of first clinical signs, versus that of repetitive dosing of these drugs on the reappearance of signs. A single shot treatment extended the period to detrimental physiological decline and death for several hours, whereas repetitive administration remained effective as long as treatment was continued. In conclusion, percutaneous VX poisoning showed to be effectively treatable when diagnosed on time and when continued over the entire period of time during which VX, in case of ineffective decontamination, penetrates the skin.
Joosen MJ, van der Schans MJ, van Helden HP. Percutaneous exposure to the nerve agent VX: Efficacy of combined atropine, obidoxime and diazepam treatment. Chem Biol Interact. 2010 Oct 6;188(1):255-63. [PubMed Citation]
-
More effective countermeasures against nerve-agent poisoning are needed, because current ones do not protect sufficiently, particularly the central nervous system (CNS). The purpose of the present study was to make a comparison of the antidotal capabilities of atropine/obidoxime/diazepam (termed the obidoxime regimen), atropine/HI-6 (1-[([4-(aminocarbonyl)pyridinio]methoxy)methyl]-2-[(hydroxyimino)methyl]pyridinium)/avizafone (termed the HI-6 regimen), and scopolamine/HI-6/physostigmine (termed the physostigmine regimen) against various doses of soman (2, 3, 4 x LD(50) ). The results showed that each regimen administered twice (1 min and 5 min after exposure) effectively prevented or terminated epileptiform activity within 10 min. However, the regimens differed markedly in life-saving properties with the physostigmine regimen ranking highest followed in descending order by the HI-6 and obidoxime regimens. Pretreatment with pyridostigmine increased the potency of the HI-6 regimen, but not the obidoxime regimen. The latter regimen administered thrice (1 min, 5 min, and 9 min after exposure) did not compensate for the insufficiency. In half of the rats that lived for 7 days, neuropathology was unexpectedly observed predominantly in the left hemisphere unrelated to whether they seized or not. Local glutamatergic excitotoxic activity may occur even if manifest toxic signs are absent. The physostigmine regimen has excellent antidotal capacity, but the very narrow therapeutic window (< 10 min) makes it unsuitable for use in the field. The HI-6 regimen appears to constitute an efficacious therapy against lower doses of soman (2 and 3 x LD(50) ).
Myhrer T, Enger S, Aas P. Determination of anti-convulsant and life-preserving capacities of three types of auto-injector therapies against soman intoxication in rats. Drug Test Anal.Drug Test Anal. 2012 Sep 13. doi:10.1002 [Epub ahead of print] [PubMed Citation]
-
The ability of obidoxime with atropine and diazepam mixture to reactivate acetylcholinesterase inhibited by the organophosphorus compound chlorfenvinphos was compared in the central nervous system and peripheral tissues of rats. The animals were intoxicated with chlorfenvinphos (6 mg/kg, p.o.) and treated immediately, 24 and 48 hrs later with obidoxime (50 mg/kg, i.p.), atropine (10 mg/kg, i.p.), and diazepam (10 mg/kg, i.p.) in a single dose, or in various combinations (with 2-3 drugs) simultaneously. Total tissue acetylcholinesterase activities were monitored at 2, 72, and 168 hrs after intoxication. Enzyme activity was determined using Ellman's colorimetric method. The results of the present study show that obidoxime administered separately and jointly with atropine and diazepam 24 hrs after intoxication was effective on reactivation of chlorfenvinphos-inhibited acetylcholinesterase in the central nervous system and in the peripheral tissues. However, the application of obidoxime alone or in combination with atropine and diazepam 48 hrs after chlorfenvinphos intoxication caused an increased unfavourable effect in rats. The results obtained also indicate an unfavourable interaction of obidoxime with diazepam in the course of chlorfenvinphos poisoning, when antidotes were administered immediately, 24 and 48 hrs after intoxication.
Raszewski G, Filip R. Correlation of therapeutic effect of obidoxime and dosing time in the acute intoxication by chlorfenvinphos in rats. Basic Clin Pharmacol Toxicol. 2009 Jul;105(1):37-45. [PubMed Citation]
Other non-clinical studies
Human non-clinical studies-
Acetylcholinesterase (AChE) reactivators are employed for the prophylaxis and treatment of intoxications with organophosphorus AChE inhibitors, including nerve agents and pesticides. For the recovery of inhibited enzyme, derivatives from the group of pyridinium or bispyridinium aldoximes (called oximes) are used. Adverse effects of these substances are not well elucidated, because of their narrow and one-shot usage. Owing to this fact, the study evaluated the influence of some currently applied oximes on human platelet aggregation in vitro. The antiplatelet activity of pralidoxime, obidoxime, HI-6, methoxime and HLo 7 was assayed in human platelet rich plasma (2.5 x 10(8) platelets ml(-1)) at a concentration of 1.35 mM. Arachidonic acid (AA), adenosine diphosphate (ADP), collagen (COL) and thrombin (TR) were used as agonists of platelet aggregation. All tested substances, except pralidoxime and methoxime, caused a significant inhibition of the aggregation process induced by AA, ADP and COL. Of the oximes assayed, none was found to influence TR triggered aggregation. Since reduced platelet aggregation can play an important role as an adverse effect in reactivator administration, further evaluation is needed for the estimation of the real impact of active oximes to the aggregation process in humans.
Jun D, Kuca K, Hronek M, Opletal L. Effect of some acetylcholinesterase reactivators on human platelet aggregation in vitro. J Appl Toxicol. 2006 May-Jun;26(3):258-61 [PubMed Citation]
-
Organophosphorus pesticides (e.g. chlorpyrifos, malathion, and parathion) and nerve agents (sarin, tabun, and VX) are highly toxic organophosphorus compounds with strong inhibition potency against two key enzymes in the human body-acetylcholinesterase (AChE; EC 3.1.1.7) and butyrylcholinesterase (BuChE; EC 3.1.1.8). Subsequent accumulation of acetylcholine at synaptic clefts can result in cholinergic crisis and possible death of intoxicated organism. For the recovery of inhibited AChE, derivatives from the group of pyridinium or bispyridinium aldoximes (called oximes) are used. Their efficacy depends on their chemical structure and also type of organophosphorus inhibitor. In this study, we have tested potency of selected cholinesterase reactivators (pralidoxime, obidoxime, trimedoxime, methoxime and H-oxime HI-6) to reactivate human erythrocyte AChE and human plasma BuChE inhibited by pesticide paraoxon. For this purpose, modified Ellman's method was used and two different concentrations of oximes (10 and 100 microM), attainable in the plasma within antidotal treatment of pesticide intoxication were tested. Results demonstrated that obidoxime (96.8%) and trimedoxime (86%) only reached sufficient reactivation efficacy in case of paraoxon-inhibited AChE. Other oximes evaluated did not surpassed more than 25% of reactivation. In the case of BuChE reactivation, none of tested oximes surpassed 12.5% of reactivation. The highest reactivation efficacy was achieved for trimedoxime (12.4%) at the concentration 100 microM. From the data obtained, it is clear that only two from currently available oximes (obidoxime and trimedoxime) are good reactivators of paraoxon-inhibited AChE. In the case of BuChE, none of these reactivators could be used for its reactivation.
Jun D, Musilova L, Kuca K, Kassa J, Bajgar J. Potency of several oximes to reactivate human acetylcholinesterase and butyrylcholinesterase inhibited by paraoxon in vitro. Chem Biol Interact. 2008 Sep 25;175(1-3):421-4. [PubMed Citation]
-
We have evaluated in vitro the potency of 23 oximes to reactivate human erythrocyte acetylcholinesterase (AChE) and plasma butyrylcholinesterase (BChE) inhibited by racemic leptophos-oxon (O-[4-bromo-2,5-dichlorophenyl]-O-methyl phenyl-phosphonate), a toxic metabolite of the pesticide leptophos. Compounds were assayed in concentrations of 10 and 100 muM. In case of leptophos-oxon inhibited AChE, the best reactivation potency was achieved with methoxime, trimedoxime, obidoxime and oxime K027. The most potent reactivators of inhibited BChE were K033, obidoxime, K117, bis-3-PA, K075, K074 and K127. The reactivation efficacy of tested oximes was lower in case of leptophos-oxon inhibited BChE.
Jun D, Musilova L, Pohanka M, Jung YS, Bostik P, Kuca K. Reactivation of human acetylcholinesterase and butyrylcholinesterase inhibited by leptophos-oxon with different oxime reactivators in vitro. Int J Mol Sci. 2010 Aug 3;11(8):2856-63 [PubMed Citation]
-
We have in vitro tested the ability of common, commercially available, cholinesterase reactivators (pralidoxime, obidoxime, methoxime, trimedoxime and HI-6) to reactivate human acetylcholinesterase (AChE), inhibited by five structurally different organophosphate pesticides and inhibitors (paraoxon, dichlorvos, DFP, leptophos-oxon and methamidophos). We also tested reactivation of human butyrylcholinesterase (BChE) with the aim of finding a potent oxime, suitable to serve as a "pseudocatalytic" bioscavenger in combination with this enzyme. Such a combination could allow an increase of prophylactic and therapeutic efficacy of the administered enzyme. According to our results, the best broad-spectrum AChE reactivators were trimedoxime and obidoxime in the case of paraoxon, leptophos-oxon, and methamidophos-inhibited AChE. Methamidophos and leptophos-oxon were quite easily reactivatable by all tested reactivators. In the case of methamidophos-inhibited AChE, the lower oxime concentration (10(-5) M) had higher reactivation ability than the 10(-4) M concentration. Therefore, we evaluated the reactivation ability of obidoxime in a concentration range of 10(-3)-10(-7) M. The reactivation of methamidophos-inhibited AChE with different obidoxime concentrations resulted in a bell shaped curve with maximum reactivation at 10(-5) M. In the case of BChE, no reactivator exceeded 15% reactivation ability and therefore none of the oximes can be recommended as a candidate for "pseudocatalytic" bioscavengers with BChE.
Jun, D, Musilova L, Musilek K, Kuca K. In vitro ability of currently available oximes to reactivate organophosphate pesticide-inhibited human acetylcholinesterase and butyrylcholinesterase. Int J Mol Sci. 2011;12(3):2077-2087. [PubMed Citation]
-
According to current knowledge, inhibition of acetylcholinesterase (AChE) is a very important toxic action of organphosphorus compounds (OP). Hence, it is obvious to follow the AChE activity in order to quantify the degree of inhibition and to assess possible reactivation. Red blood cell (RBC)-AChE provides an easily accessible source to follow the AChE status also in humans. There are many reports underlining the appropriateness of RBC-AChE as a surrogate parameter that mirrors the synaptic enzyme. With this tool at hand, we can study the kinetic parameters of inhibition, spontaneous and oxime-induced reactivation, as well as aging with human RBCs under physiological conditions in vitro. Moreover, we can simulate the influence of inhibitor and reactivator on enzyme activity and can calculate what happens when both components change with time. Finally, we can correlate under controlled conditions the AChE-status in intoxicated patients with the clinical signs and symptoms and determine the time-dependent changes of the oxime and OP concentration. Data of a clinical trial performed in Munich to analyze the value of obidoxime has elucidated that obidoxime worked as expected from in vitro studies. Following a 250 mg bolus, obidoxime was administered by continuous infusion at 750 mg/24 h aimed at maintaining a plasma concentration of 10-20 uM Mobidoxime. This oxime concentration reactivated RBC-AChE > 20% of normal in most cases of OP poisoning by diethylphosphoryl compounds within a few hours. The degree of reactivation fitted theoretical calculations very well when the obidoxime and paraoxon concentrations were fed into the model. Only in a few cases reactivation was much lower than expected. The reason for this effect is probably based on the polymorphism of paraoxonase (PON1) in that the 192arginine phenotype does hardly hydrolyze the arising diethylphosphoryl obidoxime. While this variable may complicate a proper assessment even more, we are confident that the in vitro evaluation of all relevant kinetic data enables the prediction of probable effectiveness in humans. These studies also help to understand therapeutic failures and to define scenarios where oximes are virtually ineffective. These include poisonings with rapidly aging phosphylated AChE, late start with an effective oxime and too early discontinuation of oximes in poisonings with a persistent OP. The experience gathered with the experimental and therapeutic approaches to human poisoning by OP pesticides may be helpful when oximes have to be selected against nerve agents.
Eyer P, Szinicz L, Thiermann H, Worek F, Zilker T. Testing of antidotes for organophosphorus compounds: Experimental procedures and clinical reality. Toxicology. 2007 Apr 20;233(1-3):108-19. [PubMed Citation]
-
Acetylcholinesterase was purified from human caudate nucleus and skeletal muscle. The enzyme preparations were used to study aging and reactivation by HI-6 and obidoxime after inhibition by soman and its isomers. HI-6 was found to be the most potent reactivator. For both enzyme preparations a higher reactivatability and a higher rate of aging were observed after inhibition by C+-soman than after inhibition by C(-)-soman. Aging was retarded by propidium diiodide. Reactivation by the two oximes was also studied after inhibition by tabun, sarin and VX. Tissue homogenates were used for this part of the work. Our conclusion is that HI-6 is superior to obidoxime for human acetylcholinesterases inhibited by soman and sarin, while obidoxime is better towards tabun-inhibited enzyme.
Puu G, Artursson E, Bucht G. Reactivation of nerve agent inhibited human acetylcholinesterases by HI-6 and obidoxime. Biochem Pharmacol. 1986 May 1;35(9):1505-1510. [PubMed Citation]
Comparative human and animal in vitro studies-
Previous in vitro studies showed marked species differences in the reactivating efficiency of oximes between human and animal acetylcholinesterase (AChE) inhibited by organophosphorus (OP) nerve agents. These findings provoked the present in vitro study which was designed to determine the inhibition, aging, spontaneous and oxime-induced reactivation kinetics of the pesticide paraoxon, serving as a model compound for diethyl-OP, and the oximes obidoxime, pralidoxime, HI 6 and MMB-4 with human, Rhesus monkey, swine, rabbit, rat and guinea pig erythrocyte AChE. Comparable results were obtained with human and monkey AChE. Differences between human, swine, rabbit, rat and guinea pig AChE were determined for the inhibition and reactivation kinetics. A six-fold difference of the inhibitory potency of paraoxon with human and guinea pig AChE was recorded while only moderate differences of the reactivation constants between human and animal AChE were determined. Obidoxime was by far the most effective reactivator with all tested species. Only minor species differences were found for the aging and spontaneous reactivation kinetics. The results of the present study underline the necessity to determine the inhibition, aging and reactivation kinetics in vitro as a basis for the development of meaningful therapeutic animal models, for the proper assessment of in vivo animal data and for the extrapolation of animal data to humans.
Worek F, Aurbek N, Wille T, Eyer P, Thiermann H. Kinetic analysis of interactions of paraoxon and oximes with human, Rhesus monkey, swine, rabbit, rat and guinea pig acetylcholinesterase. Toxicol Lett. 2011 Jan 15;200(1-2):19-23 [PubMed Citation]
-
Organophosphorus compounds such as nerve agents inhibit, practically irreversibly, cholinesterases by their phosphorylation in the active site of these enzymes. Current antidotal treatment used in the case of acute nerve agent intoxications consists of combined administration of anticholinergic drug (usually atropine) and acetylcholinesterase (AChE, EC 3.1.1.7) reactivator (HI-6, obidoxime, pralidoxime), which from a chemical view is a derivative from the group of pyridinium or bispyridinium aldoximes (commonly called "oxime"). Oximes counteract acetylcholine increase, resulting from AChE inhibition. In the human body environment these compounds are powerful nucleophiles and are able to break down the bond between AChE and nerve agent molecule. This process leads to renewal of enzyme functionality -- to its reactivation. The usefulness of oxime in the reactivation process depends on its chemical structure and on the nerve agent whereby AChE is inhibited. Due to this fact, selection of suitable reactivator in the treatment of intoxications is very important. In our work, we have compared differences in the in vitro inhibition potency of VX and Russian VX on rat, pig and human brain, and subsequently we have tested reactivation of rat brain cholinesterase inhibited by these agents using oxime HI-6, obidoxime, pralidoxime, trimedoxime and methoxime. The results showed that no major differences in the reactivation process of both VX and Russian VX-inhibited cholinesterase. The similarity in reactivation was caused by analogous chemical structure of either nerve agent; and that oxime HI-6 seems to be the most effective reactivator tested, which confirms that HI-6 is currently the most potent reactivator of AChE inhibited by nerve agents. The results obtained in our study should be considered in the future development of new AChE reactivators.
Kuca K, Jun D, Cabal J, Hrabinova M, Bartosova L, Opletalova V. Russian VX: inhibition and reactivation of acetylcholinesterase compared with VX agent. Basic Clin Pharmacol Toxicol. 2006 Apr;98(4):389-94. [PubMed Citation]
Animal in vitro studies-
A comparison of one mono- and seven bisquaternary acetylcholinesterase (AChE) reactivators of acetylcholinesterase inhibited by VX agent was performed. As a source of the acetylcholinesterase, a rat brain homogenate was taken. There were significant differences in reactivation potency of all tested oximes. The oxime TO205 seems to be the most efficacious followed by TO046, HI-6, HS-6, K027, obidoxime, MMC and 2-PAM. In addition, the results of this study showed that the reactivation potency of the tested reactivators depends on many factors--such as the number of pyridinium rings, the number of oxime groups and their position, as well as the length and the shape of linkage bridge between two pyridinium rings.
Kuca, K, Kassa J. Oximes-induced reactivation of rat brain acetylcholinesterase inhibited by VX agent. Hum Exp Toxicol. 2004 Apr;23(4):167-71. [PubMed Citation]
-
In our study, we have tested six acetylcholinesterase (AChE) reactivators (pralidoxime, obidoxime, HI-6, trimedoxime, BI-6 and Hlo-7) for reactivation of sarin- and cyclosarin-inhibited AChE using an in vitro reactivation test. We have used rat brain homogenate as the suitable source of enzyme. All oximes are able to reactivate sarin-inhibited AChE. On the other hand, only HI-6 is able to reactivate satisfactorily cyclosarin-inhibited AChE.
Kuca K, Cabal J, Jun D, Kassa J, Bartosová L, Kunesová G. In vitro reactivation potency of some acetylcholinesterase reactivators against sarin- and cyclosarin-induced inhibitions. J Appl Toxicol. 2005 Jul-Aug;25(4:296-300. [PubMed Citation]
-
Searching for new potent acetylcholinesterase (AChE; E.C. 3.1.1.7) reactivators (oximes) is a very time-consuming process. At our department, we are able to synthesize more than 50 new AChE reactivators per year. Owing to this fact, we have to select promising reactivators using our in vitro method (potentiometric titration, pH 8 and temperature 25 degrees C; source of cholinesterases, rat brain homogenate; time of inhibition by nerve agents, 30 min; time of reactivation, 10 min) prior to in vivo experiments. For this purpose, we are using two-phase in vitro evaluation of reactivator potency. In the first phase, reactivation potency of all newly synthesized AChE reactivators is tested at two concentrations: 10(-3) M and 10(-5) M. Afterwards, all reactivators achieving reactivation potency over 15% (especially at the concentration 10(-5) M) are tested. The second phase consists of the measurement of the relationship between concentration of the oxime and its reactivation ability. In most cases, the reactivation bell-shaped curve is obtained. The most potent AChE reactivators are selected and provided for further experiments during our development process.
Kuca K, Cabal J, Jun D, Hrabinova M. In vitro evaluation of acetylcholinesterase reactivators as potential antidotes against tabun nerve agent poisonings. Drug Chem Toxicol. 2006;29(4):443-9. [PubMed Citation]
-
The efficacy of H oximes (HI-6, HLo-7), the oxime BI-6, and currently used oximes (pralidoxime, obidoxime, trimedoxime) to reactivate acetylcholinesterase inhibited by two nerve agents (tabun, VX agent) was tested in vitro. Both H oximes (HI-6, HLo-7) and the oxime BI-6 were found to be more efficacious reactivators of VX-inhibited acetylcholinesterase than pralidoxime and obidoxime. On the other hand, their potency to reactivate tabun-inhibited acetylcholinesterase was low and did not reach the reactivating efficacy of trimedoxime and obidoxime. Thus, none of these compounds can be considered to be a broad-spectrum reactivator of nerve agent-inhibited acetylcholinesterase in spite of high potency to reactivate acetylcholinesterase inhibited by some nerve agents. More than one oxime may be necessary for the antidotal treatment of nerve agent-exposed individuals.
Kuca K, Cabal J, Kassa J, Jun D, Hrabinova M. In vitro potency of H oximes (HI-6, HLö, the oxime BI-6, and currently used oximes (pralidoxime, obidoxime, trimedoxime) to reactivate nerve agent-inhibited rat brain acetylcholinesterase. J Toxicol Environ Health A. 2006 Aug;69(15):1431-40. [PubMed Citation]
-
In vitro comparison of reactivation efficacy of five currently used oximes - pralidoxime, obidoxime, trimedoxime, methoxime, and HI-6 (at two concentrations: 10-5 and 10-3 M) - against acetylcholinesterase (AChE; E.C. 3.1.1.7) inhibited by six different nerve agents (VX, Russian VX, sarin, cyclosarin, tabun, soman) and organophosphorus insecticide chlorpyrifos was the aim of this study. As a source of AChE in the experiments, rat brain homogenate was used. According to the results obtained, no AChE reactivator was able to reach sufficient potency for AChE inhibited by all nerve agents used. Moreover, oxime HI-6 (the most effective one) was not able to reactivate tabun- and soman-inhibited AChE. Due to this fact, it could be designated as a partially broad-spectrum reactivator.
Kuca K, Jun D, Bajgar J. Currently used cholinesterase reactivators against nerve agent intoxication: comparison of their effectivity in vitro. Drug Chem Toxicol. 2007;30(1):31-40 [PubMed Citation]
-
Administration of acetylcholinesterase (AChE) reactivators (oximes) is usually used in order to counteract the poisoning effects of nerve agents. The possibility was suggested that oximes may show some therapeutic and/or adverse effects through their action in central nervous system. There are no sufficient data about interaction of oximes with monoaminergic neurotransmitter's systems in the brain. Oxime-type AChE reactivators pralidoxime, obidoxime, trimedoxime, methoxime and HI-6 were tested for their potential to affect the activity of monoamine oxidase of type A (MAO-A) and type B (MAO-B) in crude mitochondrial fraction of pig brains. The compounds were found to inhibit fully MAO-A with half maximal inhibitory concentration (IC50) of 0.375 mmol/l (pralidoxime), 1.53 mmol/l (HI-6), 2.31 mmol/l (methoxime), 2.42 mmol/l (obidoxime) and 4.98 mmol/l (trimedoxime). Activity of MAO-B was fully inhibited by HI-6 and pralidoxime only with IC50 4.81 mmol/l and 11.01 mmol/l, respectively. Methoxime, obidoxime and trimedoxime displayed non-monotonic concentration dependent effect on MAO-B activity. Because oximes concentrations effective for MAO inhibition could not be achieved in vivo at the cerebral level, we suppose that oximes investigated do not interfere with brain MAO at therapeutically relevant concentrations.
Fišar Z, Hroudová J, Korábečný J, Musílek K, Kuča K. In vitro effects of acetylcholinesterase reactivators on monoamine oxidase activity. Curr Med Chem. 2009;16(17):176-180. [PubMed Citation]
Non-clinical reviews
-
Highly toxic organophosphorus inhibitors of acetylcholinesterase referred as nerve agents are considered to be among the most dangerous chemical warfare agents. The oximes represent very important part of medical countermeasures of nerve agent poisonings. They are used to reactivate the nerve agent-inhibited acetylcholinesterase. Despite long-term research activities, there is no single, broad-spectrum oxime suitable for the antidotal treatment of poisoning with all organophosphorus agents. There are two approaches how to increase and broaden the effectiveness of antidotal treatment of poisoning with nerve agents - to develop new structural analogues of currently available oximes and/or to combine currently available or newly developed oximes. The review describes the evaluation of the potency of newly developed oximes (especially the oxime K203) or combinations of oximes to reactivate nerve agent-inhibited acetylcholinesterase and to counteract the acute toxicity of nerve agents in comparison with single commonly used oxime (obidoxime, trimedoxime or HI-6).
Kassa J, Musilek K, Karasova JZ, Kuca K, Bajgar J. Two possibilities how to increase the efficacy of antidotal treatment of nerve agent poisonings. Mini Rev Med Chem. 2012 Jan;12(1):24-34. [PubMed Citation]
-
Since the September 11, 2001, terrorist attacks in the United States, the specter of a chemical threat against civilian populations has renewed research interest in chemical warfare agents, their mechanisms of action, and treatments that reverse their effects. In this Account, we focus specifically on organophosphorus nerve agents (OPNAs). Although some OPNAs are used as pest control, the most toxic chemicals in this class are used as chemical warfare agents in armed conflicts. The acute toxicity of OPNAs results from the irreversible inhibition of acetylcholinesterase (AChE, EC 3.1.1.7) via the formation of a covalent P-O bond at the serine hydroxyl group in the enzyme active site. AChE breaks down the neurotransmitter acetylcholine at neuronal synapses and neuromuscular junctions. The irreversible inhibition of AChE causes the neurotransmitter to accumulate in the synaptic cleft, leading to overstimulation of cholinergic receptors, seizures, respiratory arrest, and death. The current treatment for OPNA poisoning combines an antimuscarinic drug (e.g., atropine), an anticonvulsant drug (e.g., diazepam), and an AChE reactivator of the pyridinium aldoxime family (pralidoxime, trimedoxime, obidoxime, HI-6, HLö-7). Because of their high nucleophilicity, oximes can displace the phosphyl group from the catalytic serine, thus restoring the enzyme's catalytic activity. During 50 years of research in the reactivator field, researchers have synthesized and tested numerous structural modifications of monopyridinium oximes and bispyridinium oximes. In the past decade, medicinal chemists have focused their research on the more efficient bispyridinium reactivators, but all known reactivators have several drawbacks. First, due to their permanent positive charge, they do not cross the blood-brain barrier (BBB) efficiently and do not readily reactivate AChE in the central nervous system. Second, no single oxime is efficient against a wide variety of OPNAs. Third, oximes cannot reactivate "aged" AChE. This Account summarizes recent strategies for the development of AChE reactivators capable of crossing the BBB. The use of nanoparticulate transport and inhibition of P-glycoprotein efflux pumps improves BBB transport of these AChE reactivators. Chemical modifications that increased the lipophilicity of the pyridinium aldoximes, the addition of a fluorine atom and the replacement of a pyridyl ring with a dihydropyridyl moiety, enhances BBB permeability. The glycosylation of pyridine aldoximes facilitates increased BBB penetration via the GLUT-1 transport system. The development of novel uncharged reactivators that can move efficiently across the BBB represents one of the most promising of these new strategies.
Mercey G, Verdelet T, Renou J, Kliachyna M, Baati R, Nachon F, Jean L, Renard PY. Reactivators of acetylcholinesterase inhibited by organophosphorus nerve agents. Acc Chem Res. 2012 May 15;45(5):756-66. [PubMed Citation]
-
During more than five decades, pyridinium oximes have been developed as therapeutic agents used in the medical treatment of poisoning with organophosphorus compounds. Their mechanism of action is reactivation of acetylcholinesterase (AChE) inhibited by organophosphorus agents. Organophosphorus compounds (OPC) are used as pesticides and developed as warfare nerve agents such as tabun, soman, sarin, VX and others. Exposure to even small amounts of an OPC can be fatal and death is usually caused by respiratory failure resulting from paralysis of the diaphragm and intercostal muscles, depression of the brain respiratory center, bronchospasm, and excessive bronchial secretions. The mechanism of OPC poisoning involves phosphorylation of the serine hydroxyl group at the active site of AChE leading to the inactivation of this essential enzyme, which has an important role in neurotransmission. AChE inhibition results in the accumulation of acetylcholine at cholinergic receptor sites, producing continuous stimulation of cholinergic fibers throughout the central and peripheral nervous systems. Presently, a combination of an antimuscarinic agent, e.g. atropine, AChE reactivator such as one of the standard pyridinium oximes (pralidoxime, trimedoxime, obidoxime, HI-6) and diazepam has been used for the treatment of organophosphate poisoning in humans. Despite enormous efforts devoted to synthesis and development of new pyridinium oximes as potential antidotes against poisoning with OPC, only four compounds have found their application in human medicine so far. However, they differ in their activity in poisoning with warfare nerve agents and pesticides and there is still no universal broad-spectrum oxime capable of protecting against all known OPC. In this article, we review data on structure-activity relationship of pyridinium oximes and discuss their pharmacological and toxicological significance.
Jokanović M, Prostran M. Pyridinium oximes as cholinesterase reactivators. Structure-activity relationship and efficacy in the treatment of poisoning with organophosphorus compounds. Curr Med Chem. 2009;16(17):2177-88. [PubMed Citation]
4. Pharmacokinetic and toxicokinetics data
— including children-, pregnancy-, geriatric-, and obesity-related dataAdult
-
OBJECTIVES: Reactivation of inhibited acetylcholinesterase (AChE) with oximes is a causal therapy of intoxication with organophosphorus compounds (OPs). Maximal oxime effects are expected when effective doses are administered as soon as possible and as long as reactivation can be anticipated. An obidoxime plasma level in the range of 10-20 microM was estimated as appropriate. The achievement of this target was assessed in 34 severely OP-poisoned patients. METHODS: After admission to the intensive care unit (ICU) the obidoxime regimen (250 mg i.v. as bolus, followed by 750 mg/24h) was started and maintained as long as reactivation was possible. Plasma concentrations of obidoxime were determined by HPLC. RESULTS: A total amount of 2269+/-1726 mg obidoxime was infused over 65 h+/-55 h resulting in a steady state plasma concentration of 14.5+/-7.3 microM. Obidoxime was eliminated with t(1/2(1)) 2.2 and t(1/2(2)) 14 h. The volumes of distribution amounted to 0.32+/-0.1L/kg (V((1))) and 0.28+/-0.12 (V((2)))L/kg. Postmortem examination of tissue in one patient showed obidoxime accumulation in cartilage, kidney and liver and pointed to brain concentrations similar to plasma concentration. CONCLUSIONS: Using the suggested obidoxime regimen, the targeted plasma concentration could be achieved. Obidoxime was eliminated biphasically and was well tolerated. This result allows the recommendation of using this definite regimen for adults also in case of mass casualties.
Thiermann H, Eyer F, Felgenhauer N, Pfab R, Zilker T, Eyer P, Worek F. Pharmacokinetics of obidoxime in patients poisoned with organophosphorus compounds. Toxicol Lett. 2010 Sep 1;197(3):236-42. [PubMed Citation]
-
Obidoxime is an oxime used in several countries as an antidote in organophosphate intoxication. Its pharmacokinetics were studied in a 20 year-old female with severe and complicated methamidophos intoxication. Obidoxime elimination half life was 6.9 h, volume of distribution 0.845 L/kg, total body clearance 85.4 mL/min, and renal clearance 69 mL/min (creatinine clearance 54 mL/min). Eighty percent of the dose was excreted in the urine over 5 h. Possible reasons for the different pharmacokinetic values as compared with values previously reported in healthy volunteers are discussed. Obidoxime dose should be adjusted according to renal function. More studies are needed to establish the therapeutic window of obidoxime in patients with organophosphate intoxication.
Bentur Y, Nutenko I, Tsipiniuk A, Raikhlin-Eisenkraft B, Taitelman U. Pharmacokinetics of obidoxime in organophosphate poisoning associated with renal failure. J Toxicol Clin Toxicol. 1993;31(2):315-22. [PubMed Citation]
-
Intoxication with organophosphorous nerve agents such as paraoxon requires immediate administration of antidotes such as oximes. However, the oximes lack sufficient activity in the central nervous system as they are unable to rapidly penetrate the blood-brain barrier (BBB) in therapeutically relevant concentrations. Human serum albumin (HSA) nanoparticles represent a promising drug carrier system for the transport of drugs across the BBB. This study focussed on the development of an obidoxime-loaded nanoparticles prepared by desolvation using an incorporation technique. The nanoparticle preparation parameters, i.e. drug amount, pH value, ethanol volume and crosslinking degree, were optimised. The in vitro release study showed a sustained release profile, indicating the suitability of the developed formulation for the transport of oximes across the BBB.
Kufleitner J, Worek F, Kreuter J. Incorporation of obidoxime into human serum albumin nanoparticles: optimisation of preparation parameters for the development of a stable formulation. J Microencapsul. 2010;27(7): 594-601. [PubMed Citation]
-
Obidoxime is an antidote approved for reactivation of inhibited acetylcholinesterase in organophosphate poisoning. HPLC methods were described for its determination in blood or aqueous solutions but not for the determination in urine. Since data for renal obidoxime excretion ranged from 2.2 to 84% of administered dose in healthy volunteers depending on the route of administration and little is known about pharmacokinetics of obidoxime in severely intoxicated patients we developed an internal standard (HI 6) reversed-phase HPLC method for determining obidoxime in urine. The mobile phase consisted of methanol, the counter ion 1-heptane sulfonic acid and tetrabutylammonium phosphate, the stationary phase involved a 5 microm reversed-phase column (125x4 mm). Obidoxime was detected spectrophotometrically at 288 nm. The limit of quantification (LOQ) was 1 microM, the limit of detection (LOD) 0.5 microM. Linear calibration curves were obtained in a concentration range from 1 to 1000 microM. Intra- and inter-day precision C.V.s were below 4%. Accuracy was 95.9% in the LOQ range. Using this method, we were able to quantify obidoxime in urine of an organophosphate poisoned patient. Based on this data we calculated that 58% of the administered dose was excreted in the urine.
Grasshoff C, Thiermann H, Gillessen T, Zilker T, Szinicz L. Internal standard high-performance liquid chromatography method for the determination of obidoxime in urine of organophosphate-poisoned patients. J Chromatogr B Biomed Sci Appl. 2001 Apr 5;753(2):203-8. [PubMed Citation]
-
In a patient who had received obidoxime for 12 days and died 15 days after parathion poisoning, obidoxime concentratons in cartilage were 100-fold higher than in plasma. These data indicate that the chondroitin sulfate-rich tissues may represent the deep 'compartment' from which pyridinium aldoximes are slowly released.
Marrs TC, Maynard RL, Sidell FR (eds). Chemical Warfare Agents Toxicology and Treatment (2nd ed). West Sussex, England: John Wiley and Sons Ltd (2007) p.305-29
Animal
-
The pharmacokinetics and pharmacodynamics of the oxime obidoxime (Toxogonin, 50 mg/kg iv) were investigated in anesthetized normal rats and in sarin-poisoned (50 micrograms/kg iv) rats. The kinetics were described by a two-compartment open model. The elimination half-life ranged from 35 min in normal rats to 86 min in sarin-poisoned rats. Obidoxime excretion occurred predominantly by the renal route, amounting to 4.6% of the administered dose in normal rats and to 0.9% in sarin-poisoned rats within the first hour of administration. The significantly diminished glomerular filtration rate confirmed the retardation of obidoxime excretion in sarin poisoning. The mean arterial blood pressure (MAP) response to obidoxime, measured in normal rats, was a transient hypotension, but to sarin an immediate hypertension. In sarin-poisoned rats the therapeutic sequence of administration of obidoxime and atropine (5 mg/kg iv) seemed to be important: the administration of atropine 10 min after and of obidoxime 20 min after sarin poisoning exerted a stabilizing effect on MAP. No serum albumin binding was found for obidoxime. Competition experiments at the isolated nicotinic receptor demonstrated the anticholinergic activity of obidoxime. The affinity of obidoxime was 1000 times smaller than that of acetylcholine. It is concluded that obidoxime, due to its prolonged residence time in the organism in sarin poisoning, exerts a "curare-like" inhibition and protection of the nicotinic acetylcholine receptor and, combined with atropine, a synergistic effect on blood pressure normalization.
Alioth-Streichenberg CM, Bodmer DM, Waser PG. Pharmacokinetics and pharmacodynamics of obidoxime in sarin-poisoned rats. Toxicol Appl Pharmacol. 1991 May;108(3):509-19. [PubMed Citation]
5. Current FDA/EUA approved indications and dosing
— including children-, pregnancy-, geriatric-, and obesity-related data, and Emergency Use Authorization (EUA)Emergency Use Authorization (FDA/CDC)
No Emergency Use Authorization for Obidoxime has been issued from the Food and Drug Administration under section 564 of the Federal Food, Drug and Cosmetic Act (FD&C Act) (21 U.S.C. 360bbb-3), amended by the Project Bioshield Act of 2004 (Public Law 108-276).
[DHHS/FDA; Emergency Preparedness and Response-Counterterrorism and Emerging Threats (12/01/2011)]
6. Current available formulations/shelf life
Shelf life
Stability
-
The degradation of obidoxime chloride (toxogonin), a reactivator of inhibited cholinesterase in organophosphorus poisoning, in concentrated (250 mg mL(-1)) acidic solutions was studied by HPLC at several temperatures to determine the degradation mechanism. The degradation had an autocatalytic profile, which was found to result from the formation of formaldehyde during the degradation process. The activation energy of the hydrolysis was 26.2 kcal mol(-1). The shelf-life (t90, the time by which 10% of the drug has degraded) at 25 degrees C was calculated by several methods and found to be more than 37 years. Autocatalysis, a mechanism found only rarely in the degradation of pharmaceuticals, has not been reported in previous studies of obidoxime hydrolysis.
Rubnov S, Shats I, Levy D, Amisar S, Schneider H. Autocatalytic degradation and stability of obidoxime. J Pharm Pharmacol. 1999 Jan;51(1):9-14. [PubMed Citation]
-
Analysis of aqueous obidoxime (250 mg ml(-1)) stored at approximately 20 deg C for 19 years yielded 92% obidoxime, 2.5% of the presumed monocarboxy derivative, 0.16% formaldehyde and only traces (0.7 ug mL(-1) of cyanide, while the pH had dropped to about 3.5.
Formation of free formaldehyde may accelerate the decomposition of obidoxime and it has been argued that formaldehyde reacting with the liberated hydroxylamine may shift the equilibrium in favour of the aldehyde and eventually to the carboxylic acid.
Marrs TC, Maynard RL, Sidell FR (eds). Chemical Warfare Agents Toxicology and Treatment (2nd ed). West Sussex, England: John Wiley and Sons Ltd (2007) p.305-29
7. Current off label utilization and dosing
— including children-, pregnancy-, geriatric-, and obesity-related data- No data available at this time.
8. Route of Administration/Monitoring
-
Obidoxime chloride is given with atropine by slow intravenous injecton. This may be followed by an intravenous infusion.
Sweetman SC (ed). Martindale, The Complete Drug Reference. London: Pharmaceutical Press (2009) p.1456
-
One-chamber Auto Injector (obidoxime chloride + atropine) is a single use device serving for automatic intramuscular injection of obidoxime and atropine. The tip of the needle is especially designed to ensure strength due to the necessity of penetration through layers of clothing.
Product Information. Obidoxime Choride/Atrophine Auto-Injector
9. Adverse effects
-
Obidoxime chloride 250 mg IM elicited adverse effects in humans, including a hot and tight feeling in the orofacial region, along with numbness. In addition, a cold sensation in the rhino-pharynegeal region was noted, similar to the effect of menthol. The symptoms usually developed within 15 minutes of injection. At a higher dose, 10 mg kg (-1) IM, a dry mouth and hot feelings in the throat were observed in all subjects who also noticed paraesthesia of variable severity. All subjects had a mild-to-moderate transient increase in systolic and diastolic blood pressure along with some tachycardia (increase in heart rate 30 pbm after 10 mg kg (-1). In another study, 11 volunteers of both sexes received obidoxime 250 mg IM to screen for possible hepatotoxicity. No abnormal liver function data were found in the 1 month follow-up period. The volunteers experienced the usual sensations as already described. In severely OP-poisoned patients treated with obidoxime, several grams per day, hepatotoxic effects were occasionally observed, including cholestasis, jaundice and elevated serum aminotransferases.
Marrs TC, Maynard RL, Sidell FR (eds). Chemical Warfare Agents Toxicology and Treatment (2nd ed). West Sussex, England: John Wiley and Sons Ltd (2007) p.305-29
-
In a recent multicenter study of severely OP-poisoned patients lead from Munich, all patients received a 250 mg obidoxime short infusion followed by continuous infusion of 750 mg obidoxime over 24 hours. No patient with dimethoate poisoning (n=6) had pathological liver pathology, while eight patients with parathion poisoning (n=13) had abnormal liver function tests. Hence, it cannot be ruled out that the type of OP and the other ingredients of the formulate may contribute to liver pathology. Cardiac arrhythmias have occasionally been associated with obidoxime therapy: 1/17 had a second-degree atrioventricluar block, with 2/17 had atrial fibrillation. We also observed some transient arrhythmias in our Munich study but did not consider these effects to be related to obidoxime.
Marrs TC, Maynard RL, Sidell FR (eds). Chemical Warfare Agents Toxicology and Treatment (2nd ed). West Sussex, England: John Wiley and Sons Ltd (2007) p.305-29
-
Twenty-four male volunteers were given obidoxime tablets in quantities ranging from 1.84-3.58 g in a single dose, or 7.36 g divided into 4 equal doses. With the lowest dose, average peak plasma level of the drug was 1.9 mug/ml and after the highest single dose it was 5.6 mug/ml, both attained 1.5 h after administration. In the multiple-dosed individuals, plasma levels of the oxime increased gradually following each additional dose, reaching a peak of 3.5 mug/ml after the last dose. Thirteen individuals complained of one or more of the following side effects: pallor, nausea, pyrosis, headache, generalized weakness, sore throat, and paresthesia of the face muscles. Activities of blood cholinesterase, glutamic oxalacetic transaminase, glutamic pyruvic transaminase, as well as hematocrit values, heart rate, and blood pressure were not affected. It is postulated that due to the undesirable side effects, the general use of obidoxime tablets should not be recommended. However, prophylactic oral treatment with obidoxime could be considered for persons at high risk of organophosphate poisoning or when parenteral administration might not be feasible.
Simon GA, Tirosh MS, Edery H. Administration of obidoxime tablets to man. Plasma levels and side reactions. Arch Toxicol. 1976 Sep 15;36(1):83-8. [PubMed Citation]
-
Oximes are generally nonlethal in the doses likely to be prescribed but do cause many mild adverse effects. Cardiovascular effects include tachycardia and mild hypertension associated with rapid injusion. ... Tachycardia and hypertension, pain at the injection site, and perioral paresthesia and methanol taste were described with toxogonin administration at doses of 2.5 to 10.0 mg/kg. Dizziness, headache, drowsiness, and apprehension associated with rapid infusion have been reported. Skin rash may occur. Gastrointesintal effects include nausea and hepatic enzyme elevation. Blurred vision, diplopia, and mydriasis have been reported. More severe reactions include apnea, hyperventilation, and laryngospasm associated with rapid infusion.
Dart RC, ed. Medical Toxicology 3rd Edition. Philadelphia, PA: Lippincott Williams & Wilkins, 2004 p.240-3
10. Contraindication(s)
- No data available at this time.
11. Clinical studies in progress
— including relevant ones and any others highlighting possible adverse effects and other effects/issues- No data available at this time.
12. Non-clinical studies in progress
— including relevant ones and any others highlighting possible adverse effects and other effects/issues-
Title: Next generation oxime therapeutic for chemical agent inhibited CNS (brain) ChEs
Current treatment of acute pesticide or organophosphate (OP) poisoning includes a combined administration of a cholinesterase reactivator (oxime), a muscarinic receptor antagonist (atropine) and an anticonvulsant (diazepam). Since the oxime does not penetrate the blood brain barrier (BBS), removal of excessive accumulation of acetylcholine (ACh) is not accomplished by acetylcholinesterase (AChE). Pesticides and OPs are significant terrorist threats to civilian populations. The chemical agent sarin was used in the Tokyo subway terrorist event in 1995 and resulted in long-term neuronal sequelae. Clearly, a new formulation of oxime is required to improve CNS therapy. Because of their chemical structure, the positively charged small molecule oximes do not penetrate the BBB and therefore can not treat pesticide- and OP- induced toxicity in the brain. The long term goal is to transport oxime (2-PAM, MMB-4) quickly and non-invasively into the CNS. CNS-penetrating oxime therapy will reactivate the brain AChE in a timely manner, reduce the requirement for anticonvulsant drug regimens, and improve the long term recovery of the exposed individual by reducing or eliminating CNS neuronal damage, (a) The investigators will synthesize and evaluate more lipoidal forms (pro-oximes), that can be converted to their active (charged) form in the brain, (b) In addition, the investigators will develop carrier(s) of oximes that will come from a class of FDA approved/phase 1 trial Pharmaceuticals that pass the BBB... including Stealth liposomes, nanoparticles, or cyclodextrins. (c) Two additional advantages to the carriers: should permit a sustained delivery of oxime into the systemic circulation through the skin (via skin patch) and prolong the circulatory time of the oxime(s), which are rapidly cleared by the renal system (T1/2<2 hr). (d) For formulations that are successful in in vitro BBB tissue culture and pig skin penetration models, the investigators will determine reactivation kinetics of the encapsulated oximes with pesticide- and OP-inhibited AChE and BuChE, the release rates of the oxime from the carrier in the peripheral and CNS of animal model (guinea pig), and the pharmacokinetics of the pro-oxime and oxime carrier and distribution in diaphragm, blood, and brain, (d) The most efficacious formulation will be validated in a status epilepticus guinea pig model as a therapy for CNS chemical agent OP-induced toxicity of DFP, GB, GD, and VX using EEC radiotelemetry probe techniques. This program will address an important and potential threat to civilian populations, for post-exposure CNS treatment in response to exposure to chemical threat agents. Further, the outcome of this work could provide a non-invasive means of administrating appropriate therapeutics for deleterious effects of OP poisoning, directly relevant to emergency and preparedness response to chemical threats for Public Health.
RePORTER. NIH. Next generation oxime therapeutic for chemical agent inhibited CNS (brain) ChEs.
-
Title: Rapid development of in vivo models for countermeasure discovery: organophosphate
A major problem in chemical countermeasure discovery is the potential emergence of novel agents for which there are no known antidotes or post exposure therapies. Classic countermeasures have often been discovered only serendipitously or have taken years to develop. As novel chemical threats emerge (in the form of novel chemical warfare agents or environmental pollutants), the speed with which we are able to understand and counteract each threat will determine the magnitude of its societal impact. One promising approach for rapidly identifying and manipulating the molecular pathways underlying the response to any chemical threat is the use of phenotype-based chemical screens. Models can be developed in which specific toxicants result in reproducible phenotypes in cells or whole organisms. By subjecting these models to high-throughput screening (HTS), small molecules could be identified that reverse the phenotype through a variety of novel mechanisms. Small molecules discovered by these screens would be excellent lead compounds for novel countermeasures and powerful tools for dissecting toxicity pathways, which may in turn point to additional countermeasure targets. In this application, the investigators outline a process for rapid development of in vivo organophosphate toxicity models and their use in discovery of novel organophosphate countermeasures. Although the investigators expect the proposed project will lead directly to development of novel organophosphate countermeasures, they also expect it to serve as a model for rapid countermeasure development that can be applied broadly to other existing and emerging chemical threats. Specifically, the investigators propose: Aim 1. To develop and validate in vivo assays for organophosphate toxicity in the zebrafish. They will seek to identify physiological responses that are surrogates for known human responses to organophosphates and that can be scaled for high throughput in vivo screening. Aim 2. To scale these novel assays for automated high-throughput screening in multiwell plates. The investigators will develop assays for organophosphate toxicity that can be performed automatically in 96-well format. Aim 3. To identify novel compounds that counteract the effects of prior organophosphate exposure. High-throughput screening will identify compounds that facilitate recovery from organophosphate exposure
RePORTER. NIH. Rapid development of in vivo models for countermeasure discovery: organophosphate.
-
Title: Oxime-assisted catalysis of organophosphates and reactivation of AChE
The proposed project is directed to improving prophylaxis and therapy for organophosphate nerve agent organophosphate exposure through the design of mutant human acetylcholinesterases (AChEs), novel oximes and related reactivating nucleophiles. This strategy of oxime-assisted catalysis modifies AChE such that, when placed in the circulation, the oxime and AChE become a catalytic, rather than a stoichiometric, scavenger of organophosphates. Proof of principle has already been established for hydrolysis of a series of organophosphates, and the investigators will refine AChE mutations and oxime structure to enhance catalytic rates for hydrolysis and retention in plasma space. Since oxime therapy, 2-PAM and HI-6, also reactivates inhibited AChE at the target site and the therapeutic benefits of long term oxime therapy have become fully appreciated recently, the investigators propose to design new reactivators based on contemporary knowledge of AChE structure to which they and other groups have contributed to over the past two decades. This approach considers impaction of the active center gorge and angle of access of the oxime as limiting constraints in the design strategy. Moreover, the /research/ groups have applied a novel freeze-frame, click chemistry to the development of reactivating agents using AChE-phosphonate conjugates as the template for synthesis of the triazoles. In addition to oxime assisted catalysis in plasma, new oximes and other nucleophiles will be developed as novel reactivating agents at the target site. This chemistry also enjoys the advantage of combinatorial screening for medium to high throughput in the synthesis-screening paradigm. Nucleophiles and nucleophile AChE combinations will be optimized for enhancing therapeutic efficacy to the particular offending organophosphate. Hence, the investigators approach will both augment catalytic scavenging of organophosphates in the circulation and enhance reactivation at the target tissues.
RePORTER. NIH. Oxime-assisted catalysis of organophosphates and reactivation of AChE.
-
Title: Synthesis of methylating ligands that reactivate aged acetylcholinesterase
Organophosphorus (OP) chemical warfare agents, such as sarin and soman, are acutely toxic compounds that act by inhibiting the activity of the enzyme acetylcholinesterase (AChE) at nerve-nerve and neuromuscular junctions in the central and peripheral nervous systems, respectively. Inhibition of the enzyme occurs by phosphylation of the active site serine nucleophile that is normally involved in catalysis. Prompt administration of oximes can lead to dephosphylation of the phosphyl-AChE adduct and hence is an antidote strategy. However, and particularly with the chemical warfare agent soman, the initial phosphyl-AChE adduct undergoes a dealkylation reaction that leads to what is called the aged adduct, for which there is no known antidote. This application proposes to address this perplexing problem by synthesis and evaluation of AChE ligands that can bind in the active site of the aged enzyme adduct, and subsequently serve as methyl transfer agents to realkylate the aged enzyme. This in turn will resurrect the susceptibility of the adduct to nucleophilic dephosphylation by oximes and hence lead to recovery of enzyme activity. Success in this endeavor should therefore open the door to the development of efficacious drugs for antidote therapy against currently intractable OP chemical warfare agents. PUBLIC HEALTH RELEVANCE: This application endeavors to synthesize and evaluate ligands of the enzyme acetylcholinesterase that can serve as antidotes against organophosphorus (OP) chemical warfare agents. This work is motivated by the concern that terrorist organizations may aspire to inflict mass casualties by use of these agents. It is anticipated that as OP agent antidote therapy improves, the health and security risks that these agents pose to our society will be ameliorated.
RePORTER. NIH. Synthesis of methylating ligands that reactivate aged acetylcholinesterase.
-
Title: Optimization of nonpyridinium oximes for BChE hydrolysis of OPs in plasma
The principal aim of this study is to optimize the efficient and affordable butyrylcholinesterase (BChE) based catalytic scavenger system developed in vitro for treatment of acute organophosphate (OP) intoxication. Currently used oxime and atropine combination therapy is inefficient for treatment of higher exposure OP poisoning due to constant acetylcholinesterase (AChE) reinhibition by excess OP. Novel approaches in therapy based on BChE as stoichiometric scavenger appear prohibitively expensive with a four figure price tag per single application. Conversion of BChE from stoichiometric to catalytic scavenger by combining it with an oxime reactivator has been hampered by lack of efficient BChE reactivators. In the investigators preliminary studies they were able to identify a novel class of superior specific BChE reactivators of distinct nontraditional structural scaffold. The proposed study deals with optimization of this novel class of reactivators using six step optimization iterative cycle that include detailed kinetic characterization of both reactivation and OP hydrolytic properties of oxime/BChE catalytic scavenger systems in buffer medium, extracorporeal human blood and in vivo in mouse animal model. Results of preliminary studies indicate that BChE in combination with optimized oxime reactivators should completely and rapidly, in a several minute timeframe, hydrolyze OPs in plasma space following exposure to an order of magnitude higher than LD50 OP doses at a fraction of cost of currently developed BChE based stoichiometric scavenger system. The proposed optimized catalytic scavenger system technology will thus enable an effective treatment of large OP intoxicated populations and serve as deterrent to the use of OP based nerve agents as terrorist or combat weapons in closed ventilation systems. PUBLIC HEALTH RELEVANCE: This project will develop optimized, efficient and affordable butyrylcholinesterase based catalytic scavenger system for rapid degradation of toxicants in the plasma space of patients exposed to OP agents.
RePORTER. NIH. Optimization of nonpyridinium oximes for BChE hydrolysis of OPs in plasma.
13. Needed studies for Chemical Defense clinical indication
— including pharmacokinetics, safety, efficacy, pregnancy, breastfeeding, and review panel recommendations-
The development of promising scavenger molecules effective against a wide variety of chemical nerve agents should be pursued.
-
The development of oximes that are broader acting than 2-PAM, and have the ability to reverse the permanent binding that can occur with some nerve agents should be pursued.
-
Critical nerve agent antidotes should be evaluated to determine if they can be safely and effectively administered to infants, children and adults via the intravenous and aerosol routes.
-
The accelerated development of promising antidotes for chemical nerve agents should be pursued.
-
Expanded labeling of currently licensed anticonvulsants for use against chemical nerve agents and their utilization in autoinjectors should be pursued.
-
Objective screening tests that can evaluate behavior and cognitive ability, and can differentiate chemically-induced neurological injury from pre-existing neurological illness need to be developed.
Summary of the NIAID Expert Panel Review on Medical Chemical Defense Research, March 19, 2003, Bethesda, MD (NIH/NIAID)
14. Needed studies for non Chemical Defense clinical indications
— including review panel recommendations- No data available at this time.
15. Study-related ethical concerns
— including review panel recommendations- No data available at this time.
16. Global regulatory status
U.S.
-
Alternative oximes, such as trimedoxime (TMB4), Toxogonin, and HI-6 (an H-series oxime), are available in other countries for the treatment of nerve agent-induced injuries. Some of these have been or are in the process of being evaluated for use by the U.S. military, but none have been evaluated for possible use in U.S. civilian populations. Several promising new oxime candidates also have been identified and will require further investigation.
Medical Countermeasures Against Chemical Threats: Nervous System, Potential Medical Countermeasures (NIAID)
E.U.
-
In Europe, several oximes are presently available including various salts of pralidoxime as well as obidoxime. The different oximes do not have the same efficacy regarding the different nerve agents as well as the various insecticides. Thus, efficacy of oximes remains a matter of debate. The efficacy of oximes depends on (1) the chemical structure of the organophophosaphte, (2) the delay in treatment due to the ageing of the phosphorylated enzyme, (3) the endpoints used to assess their efficacy. While atropine should be immediately available at the scene of the event, oximes should be available as soon as possible. Following are the recommendations for obidoxime:
-
Adults: Initiate as soon as possible; slow IV or IM 250 m g. Repeat after 2 hours. Continuation up to 24 hours 750-1250 mg. Treatment may be needed for several days, especially for highly toxic OP.
-
Children: Initiate as soon as possible; slow IV or IM, 4-8 mg/kg (max 250 mg). Continuation of infusion of 750-1250 mg/kg for up to 24 hours.
Treatment may be needed for several days, especially for highly toxic OP.
EMEA/CPMP Guidance Document on the use of Medicinal Products for the Treatment of Patients Exposed to Terrorist Attacks with Chemical Agents (April 2003) (EMA)
Other
-
Obidoxime chloride is a cholinesterase reactivator with similar actions and uses to pralidoxime. It is given with atropine in the treatment of organophosphorus poisoning in a usual initial dose of 250 mg (4 mg/kg) by slow intravenous injection. This may be followed by intravenous infusion of 750 mg over 24 hours, continued until the concentration of organophosphate is below critical levels; alternatively, repeated doses of 4 to 8 mg/kg may be given at intervals of 2 to 4 hours. It has also been given by intramuscular injection.
Preparations: Toxogonin (Austria, Chile, Czechoslovakia, Germany, Netherlands, South Africa, Sweden, Switzerland)
Sweetman SC (ed). Martindale, The Complete Drug Reference. London: Pharmaceutical Press (2009) p.1456
-
Obidoxime Choride/Atrophine Auto-Injector
One-chamber Auto Injector (Obidoxime Chloride + Atropine) - counteraction to phosphoroorganic Toxic Warfare Agents, such as: sarin, tabun, VX, etc. The Auto Injector is a single use device serving for automatic intramuscular injection of obidoxime and atropine. The tip of the needle is specially designed to ensure strength due to the necessity of penetration through layers of clothing.
Obidoxime Chloride - The Auto Injector (220 mg per unit) delivers: obidoxime chloride - 110 mg; methyl 4-hydroxybenzoate - 0.325 mg; propyl 4-hydroxybenzoate - 0.175 mg; water for injection - at 1 ml.
Atropine Sulphate - Auto Injector delivers 2 mg of atropine in 0.7 ml of sterile pyrogen-free solution containing glycerin, phenol, citrate buffer and water for injection. The pH range is 2.8-4.5.
Product Information. Obidoxime Choride/Atrophine Auto-Injector
17. Other potentially useful information
-
The pertinent threat of using organophosphorus compound (OP)-type chemical warfare agents (nerve agents) during military conflicts and by non-state actors requires the continuous search for more effective medical countermeasures. OP inhibit acetylcholinesterase (AChE) and therefore standard treatment of respective poisoning includes AChE reactivators (oximes) in combination with antimuscarinic agents. Hereby, standard oximes, 2-PAM and obidoxime, are considered to be rather insufficient against various nerve agents. Numerous experimental oximes have been investigated in the last decades by in vitro and in vivo models. Recently, we studied the reactivating potency of several oximes with human AChE inhibited by structurally different OP and observed remarkable differences depending on the OP and oxime. In order to investigate structure-activity relationships we determined the various kinetic constants (inhibition, reactivation, aging) for a series of sarin analogues bearing a methyl, ethyl, n-propyl, n-butyl, i-propyl, i-butyl, cyclohexyl or pinacolyl group with human AChE and BChE. The rate constants for the inhibition of human erythrocyte AChE and plasma BChE by these OP (k(i)), for the spontaneous dealkylation (k(a)) and reactivation (k(s)) of OP-inhibited AChE and BChE as well as for the oxime-induced reactivation of OP-inhibited AChE and BChE by the oximes obidoxime, 2-PAM, HI 6, HLö 7 and MMB-4 were determined. With compounds bearing a n-alkyl group the inhibition rate constant increased with chain length. A relation between chain length and spontaneous reactivation velocity was also observed. In contrast, no structure-activity dependence could be observed for the oxime-induced reactivation of AChE and BChE inhibited by the compounds tested. In general, OP-inhibited AChE and BChE were susceptible towards reactivation by oximes. HLö 7 was the most potent reactivator followed by HI 6 and obidoxime while 2-PAM and MMB-4 were rather weak reactivators. These data indicate a potential structure-activity relationship concerning inhibition and spontaneous reactivation but not for oxime-induced reactivation.
Bartling A, Worek F, Szinicz L, Thiermann H. Enzyme-kinetic investigation of different sarin analogues reacting with human acetylcholinesterase and butyrylcholinesterase. Toxicology. 2007 Apr 20;233(1-3):166-72. [PubMed Citation]
-
Organophosphorus compound-based (OP) chemical warfare agents (nerve agents) represent a continuing threat to military forces and the civilian population. OPs act primarily by inhibiting acetylcholinesterase (AChE), the standard treatment for which includes AChE reactivators (oximes) in combination with antimuscarinic drugs. In the last decades, the efficacy of oximes has been investigated mostly in small animal models. In order to increase the predictive value of animal studies it is desirable to measure numerous physiological and biochemical parameters. This is difficult in small animals. Large animal models fulfil these requirements and swine are increasingly being used in toxicology studies. Swine breeds generally show considerable variability in different characteristics which may be minimised by the use of specially bred minipigs which have a known genetic background and health status. A comparative study was, therefore, initiated to investigate the kinetic properties of the White Landrace pig and Göttingen minipig AChE in respect of inhibition by the pesticide paraoxon; the nerve agents cyclosarin, VX and VR; the reactivation of inhibited AChE by oximes (obidoxime, pralidoxime and HI 6); and the aging and spontaneous reactivation of inhibited AChE. The determination of the respective kinetic constants found similarities between pig and minipig AChE which showed marked differences in comparison with human AChE values. This has to be considered in designing meaningful models for the investigation of oxime efficacy in pig or minipig experiments. The generated data indicate comparable kinetic properties of pig and minipig AChE and may provide a kinetic basis for extrapolation of data from pig studies to humans.
Worek F, Aurbek N, Wetherell J, Pearce P, Mann T, Thiermann H. Inhibition, reactivation and aging kinetics of highly toxic organophosphorus compounds: pig versus minipig acetylcholinesterase. Toxicology. 2008 Feb 3;244(1):35-41. [PubMed Citation]
-
The aim of our study was to evaluate the impact of acetylcholinesterase reactivators--K027 [1-(4-carbamoyl pyridinium)-3-(4-hydroxyiminomethyl pyridinium) propane dibromide], HI-6 [1-(4-carbamoylpyridinium)-3-(2-hydroxyimino methylpyridinium) oxapropane dichloride] and obidoxime [1,3-bis(4-hydroxyiminomethyl pyridinium)oxapropane dichloride] on hepatic functions in vivo. Male Wistar rats were randomly divided to seven groups and intramuscularly administered with saline and acetylcholinesterase reactivators (K027, HI-6 and obidoxime) at doses of 5% LD(50) and 50% LD(50). Liver tissue samples were taken 24 hr after administration. Histochemical detection of lipid droplets and immunohistochemical detection of multidrug resistance protein 2 (Mrp2) were provided. Lipid droplet count in rat liver did not show any significant differences in animals administered with K027, HI-6 and obidoxime in comparison with the control group. Mrp2 protein expression significantly decreased when animals were administered with K027 at a dose of 50% LD(50) and HI-6 and obidoxime at doses of 5% LD(50) and 50% LD(50), when compared to the controls. No statistical differences of Mrp2 expression were measured when animals were administered with K027 at a dose of 5% LD(50) in comparison with control animals. We found impaired hepatic transporter function after administration of HI-6, obidoxime and higher concentration of K027, which might be the underlying mechanism of acetylcholinesterase reactivators' hepatotoxicity.
Pejchal J, Osterreicher J, Kuca K, Jun D, Bajgar J, Kassa J. The influence of acetylcholinesterase reactivators on selected hepatic functions in rats. Basic Clin Pharmacol Toxicol. 2008 Aug;103(2):119-23. [PubMed Citation]
-
Oximes are important in the treatment of organophosphate (OP) poisoning, but have limited biological half-lives. Complexing these drugs with a macromolecule, such as a dendrimer, could improve their pharmacokinetics. The present study investigates the intermolecular interactions that drive the complexation of oxime-based drug molecules with fifth generation poly(amidoamine) (PAMAM) dendrimers. We performed steady-state binding studies of two molecules, pralidoxime and obidoxime, employing multiple NMR methods, including 1D titration, (1)H-(1)H 2D spectroscopy (COSY, NOESY), and (1)H diffusion-ordered spectroscopy (DOSY). Several important insights were gained in understanding the host-guest interactions occurring between the drug molecules and the polymer. First, the guest molecules bind to the dendrimer macromolecule through a specific interaction rather than through random, hydrophobic encapsulation. Second, this specificity is driven primarily by the electrostatic or H-bond interaction of the oxime at a dendrimer amine site. Also, the average strength for each drug and dendrimer interaction is affected by the surface modification of the polymer. Third, individual binding events between oximes and a dendrimer have a negative cooperative effect on subsequent oxime binding. In summary, this report provides a novel perspective important for designing host systems for drug delivery.
Choi SK, Thomas TP, Leroueil P, Kotlyar A, Van Der Spek AF, Baker JR Jr. Specific and Cooperative Interactions between Oximes and PAMAM Dendrimers As Demonstrated by (1)H NMR Study. J Phys Chem B. 2012 Aug 21. [Epub ahead of print] [PubMed Citation]
-
Administration of oxime therapy is currently the standard approach used to reverse the acute toxicity of organophosphorus (OP) compounds, which is usually attributed to OP inhibition of acetylcholinesterase (AChE). Rate constants for reactivation of OP-inhibited AChE by even the best oximes, such as HI-6 and obidoxime, can vary >100-fold between OP-AChE conjugates that are easily reactivated and those that are difficult to reactivate. To gain a better understanding of this oxime specificity problem for future design of improved reactivators, we conducted a QSAR analysis for oxime reactivation of AChE inhibited by OP agents and their analogues. Our objective was to identify common mechanism(s) among OP-AChE conjugates of phosphates, phosphonates and phosphoramidates that result in resistance to oxime reactivation. Our evaluation of oxime reactivation of AChE inhibited by a sarin analogue, O-methyl isopropylphosphonofluoridate, or a cyclosarin analogue, O-methyl cyclohexylphosphono fluoridate, indicated that AChE inhibited by these analogues was at least 70-fold more difficult to reactivate than AChE inhibited by sarin or cyclosarin. In addition, AChE inhibited by an analogue of tabun (i.e., O-ethyl isopropylphosphonofluoridate) was nearly as resistant to reactivation as tabun-inhibited AChE. QSAR analysis of oxime reactivation of AChE inhibited by these OP compounds and others suggested that the presence of both a large substituent (i.e., the size of dimethylamine) and an alkoxy substituent in the structure of OP compounds is the common feature that results in resistance to oxime reactivation of OP-AChE conjugates whether the OP is a phosphate, phosphonate or phosphoramidate.
Maxwell DM, Brecht KM, Sweeney RE. A common mechanism for resistance to oxime reactivation of acetylcholinesterase inhibited by organophosphorus compounds. Chem Biol Interact. 2012 Sep 12. pii: S0009-2797(12)00162-7. doi: 10.106/j.cbi.2012.08.024. [Epub ahead of print] [PubMed Citation]
-
LogP (octanol-water) = -1.990 (est)
US NLM. ChemIDplus Lite. Obidoxime
18. Publications
Aas P. In vitro effects of toxogonin, HI-6 and HLö-7 on the release of [3H]acetylcholine from peripheral cholinergic nerves in rat airway smooth muscle. Eur J Pharmacol. 1996 Apr 22;301(1-3):59-66. [PubMed Citation]
Alioth-Streichenberg CM, Bodmer DM, Waser PG. Pharmacokinetics and pharmacodynamics of obidoxime in sarin-poisoned rats. Toxicol Appl Pharmacol. 1991 May;108(3):509-19. [PubMed Citation]
Antonijevic B, Stojiljkovic MP. Unequal efficacy of pyridinium oximes in acute organophosphate poisoning. Clin Med Res. 2007 Mar;5(1):71-82. [PubMed Citation]
Balali-Mood M, Shariat M. Treatment of organophosphate poisoning. Experience of nerve agents and acute pesticide poisoning on the effects of oximes. J Physiol Paris 1998 Oct-Dec;92(5-6):375-8 [PubMed Citation]
Bartling A, Worek F, Szinicz L, Thiermann H. Enzyme-kinetic investigation of different sarin analogues reacting with human acetylcholinesterase and butyrylcholinesterase. Toxicology. 2007 Apr 20;233(1-3):166-72. [PubMed Citation]
Bartosova L, Kuca K, Jun D, Kunesova G. Bispyridinium oximes as antidotal treatment of cyclosarin poisoning-in vitro and in vivo testing. Int J Toxicol. 2005 Nov-Dec;24(6):399-402. [PubMed Citation]
Bentur Y, Nutenko I, Tsipiniuk A, Raikhlin-Eisenkraft B, Taitelman U. Pharmacokinetics of obidoxime in organophosphate poisoning associated with renal failure. J Toxicol Clin Toxicol. 1993;31(2):315-22. [PubMed Citation]
Choi SK, Thomas TP, Leroueil P, Kotlyar A, Van Der Spek AF, Baker JR Jr. Specific and Cooperative Interactions between Oximes and PAMAM Dendrimers As Demonstrated by (1)H NMR Study. J Phys Chem B. 2012 Aug 21. [Epub ahead of print] [PubMed Citation]
Dart RC, ed. Medical Toxicology 3rd Edition. Philadelphia, PA: Lippincott Williams & Wilkins, 2004 p.240-3
DHHS/FDA; Emergency Preparedness and Response-Counterterrorism and Emerging Threats (12/01/2011)
El-Naggar Ael-R, Abdalla MS, El-Sebaey AS, Badawy SM. Clinical findings and cholinesterase levels in children of organophosphates and carbamates poisoning. Eur J Pediatr. 2009 Aug;168(8):951-6. Epub 2008 Nov 8. [PubMed Citation]
EMEA/CPMP Guidance Document on the use of Medicinal Products for the Treatment of Patients Exposed to Terrorist Attacks with Chemical Agents (April 2003) (EMA)
Eyer P, Szinicz L, Thiermann H, Worek F, Zilker T. Testing of antidotes for organophosphorus compounds: Experimental procedures and clinical reality. Toxicology. 2007 Apr 20;233(1-3):108-19. [PubMed Citation]
Eyer F, Worek F, Eyer P, Felgenhauer N, Haberkorn M, Zilker T, Thiermann H. Obidoxime in acute organophosphate poisoning: 1 - clinical effectiveness. Clin Toxicol (Phila). 2009 Sep;47(8):798-806. [PubMed Citation]
Finkelstein Y, Kushnir A, Raikhlin-Eisenkraft B, Taitelman U. Antidotal therapy of severe acute organophosphate poisoning: a multihospital study. Neurotoxicol Teratol. 1989 Nov-Dec;11(6):593-6. [PubMed Citation]
Fišar Z, Hroudová J, Korábečný J, Musílek K, Kuča K. In vitro effects of acetylcholinesterase reactivators on monoamine oxidase activity. Curr Med Chem. 2009;16(17):176-180. [PubMed Citation]
Grasshoff C, Thiermann H, Gillessen T, Zilker T, Szinicz L. Internal standard high-performance liquid chromatography method for the determination of obidoxime in urine of organophosphate-poisoned patients. J Chromatogr B Biomed Sci Appl. 2001 Apr 5;753(2):203-8. [PubMed Citation]
Herkert NM, Freude G, Kunz U, Thiermann H, Worek F. Comparative kinetics of organophosphates and oximes with erythrocyte, muscle and brain acetylcholinesterase. Toxicol Lett. 2012 Mar 7;209(2):173-8. [PubMed Citation]
Jokanović M, Stojiljković MP. Current understanding of the application of pyridinium oximes as cholinesterase reactivators in treatment of organophosphate poisoning. Eur J Pharmacol. 2006 Dec 28;553(1-3):10-7. [PubMed Citation]
Jokanović M, Prostran M. Pyridinium oximes as cholinesterase reactivators. Structure-activity relationship and efficacy in the treatment of poisoning with organophosphorus compounds. Curr Med Chem. 2009;16(17):2177-88. [PubMed Citation]
Joosen MJ, van der Schans MJ, van Helden HP. Percutaneous exposure to the nerve agent VX: Efficacy of combined atropine, obidoxime and diazepam treatment. Chem Biol Interact. 2010 Oct 6;188(1):255-63. [PubMed Citation]
Jun D, Kuca K, Hronek M, Opletal L. Effect of some acetylcholinesterase reactivators on human platelet aggregation in vitro. J Appl Toxicol. 2006 May-Jun;26(3):258-61 [PubMed Citation]
Jun D, Musilova L, Kuca K, Kassa J, Bajgar J. Potency of several oximes to reactivate human acetylcholinesterase and butyrylcholinesterase inhibited by paraoxon in vitro. Chem Biol Interact. 2008 Sep 25;175(1-3):421-4. [PubMed Citation]
Jun D, Musilova L, Pohanka M, Jung YS, Bostik P, Kuca K. Reactivation of human acetylcholinesterase and butyrylcholinesterase inhibited by leptophos-oxon with different oxime reactivators in vitro. Int J Mol Sci. 2010 Aug 3;11(8):2856-63. [PubMed Citation]
Jun, D, Musilova L, Musilek K, Kuca K. In vitro ability of currently available oximes to reactivate organophosphate pesticide-inhibited human acetylcholinesterase and butyrylcholinesterase. Int J Mol Sci. 2011;12(3):2077-2087. [PubMed Citation]
Kassa J. Review of oximes in the antidotal treatment of poisoning by organophosphorus nerve agents. J Toxicol Clin Toxicol. 2002;40(6):803-16. [PubMed Citation]
Kassa J, Karasova JZ, Pavlikova R, Misik J, Caisberger F, Bajgar J. The influence of combinations of oximes on the reactivating and therapeutic efficacy of antidotal treatment of tabun poisoning in rats and mice. J Appl Toxicol. 2010 Mar;30(2):120-4. [PubMed Citation]
Kassa J, Musilek K, Karasova JZ, Kuca K, Bajgar J. Two possibilities how to increase the efficacy of antidotal treatment of nerve agent poisonings. Mini Rev Med Chem. 2012 Jan;12(1):24-34. [PubMed Citation]
Kuca, K, Kassa J. Oximes-induced reactivation of rat brain acetylcholinesterase inhibited by VX agent. Hum Exp Toxicol. 2004 Apr;23(4):167-71. [PubMed Citation]
Kuca K, Cabal J, Jun D, Kassa J, Bartosová L, Kunesová G. In vitro reactivation potency of some acetylcholinesterase reactivators against sarin- and cyclosarin-induced inhibitions. J Appl Toxicol. 2005 Jul-Aug;25(4:296-300. [PubMed Citation]
Kuca K, Cabal J, Jun D, Hrabinova M. In vitro evaluation of acetylcholinesterase reactivators as potential antidotes against tabun nerve agent poisonings. Drug Chem Toxicol. 2006;29(4):443-9. [PubMed Citation]
Kuca K, Cabal J, Kassa J, Jun D, Hrabinova M. In vitro potency of H oximes (HI-6, HLö, the oxime BI-6, and currently used oximes (pralidoxime, obidoxime, trimedoxime) to reactivate nerve agent-inhibited rat brain acetylcholinesterase. J Toxicol Environ Health A. 2006 Aug;69(15):1431-40. [PubMed Citation]
Kuca K, Jun D, Cabal J, Hrabinova M, Bartosova L, Opletalova V. Russian VX: inhibition and reactivation of acetylcholinesterase compared with VX agent. Basic Clin Pharmacol Toxicol. 2006 Apr;98(4):389-94. [PubMed Citation]
Kuca K, Jun D, Bajgar J. Currently used cholinesterase reactivators against nerve agent intoxication: comparison of their effectivity in vitro. Drug Chem Toxicol. 2007;30(1):31-40 [PubMed Citation]
Kufleitner J, Worek F, Kreuter J. Incorporation of obidoxime into human serum albumin nanoparticles: optimisation of preparation parameters for the development of a stable formulation. J Microencapsul. 2010;27(7): 594-601. [PubMed Citation]
Lifshitz M, Rotenberg M, Sofer S, Tamiri T, Shahak E, Almog S. Carbamate poisoning and oxime treatment in children: a clinical and laboratory study. Pediatrics. 1994 Apr;93(4):652-5. [PubMed Citation]
Marrs TC, Rice P, Vale JA. The role of oximes in the treatment of nerve agent poisoning in civilian casualties. Toxicol Rev. 2006;25(4): 297-323. [PubMed Citation]
Marrs TC, Maynard RL, Sidell FR (eds). Chemical Warfare Agents Toxicology and Treatment (2nd ed). West Sussex, England: John Wiley and Sons Ltd (2007) p.305-29
Maxwell DM, Brecht KM, Sweeney RE. A common mechanism for resistance to oxime reactivation of acetylcholinesterase inhibited by organophosphorus compounds. Chem Biol Interact. 2012 Sep 12. pii: S0009-2797(12)00162-7. doi: 10.1016/j.cbi.2012.08.024. [Epub ahead of print] [PubMed Citation]
Medical Countermeasures Against Chemical Threats: Nervous System, Potential Medical Countermeasures (NIAID)
Mercey G, Verdelet T, Renou J, Kliachyna M, Baati R, Nachon F, Jean L, Renard PY. Reactivators of acetylcholinesterase inhibited by organophosphorus nerve agents. Acc Chem Res. 2012 May 15;45(5):756-66. [PubMed Citation]
Myhrer T, Enger S, Aas P. Determination of anti-convulsant and life-preserving capacities of three types of auto-injector therapies against soman intoxication in rats. Drug Test Anal.Drug Test Anal. 2012 Sep 13. doi:10.1002 [Epub ahead of print] [PubMed Citation]
Pejchal J, Osterreicher J, Kuca K, Jun D, Bajgar J, Kassa J. The influence of acetylcholinesterase reactivators on selected hepatic functions in rats. Basic Clin Pharmacol Toxicol. 2008 Aug;103(2):119-23. [PubMed Citation]
Product Information. Obidoxime Choride/Atrophine Auto-Injector
Puu G, Artursson E, Bucht G. Reactivation of nerve agent inhibited human acetylcholinesterases by HI-6 and obidoxime. Biochem Pharmacol. 1986 May 1;35(9):1505-1510. [PubMed Citation]
Raszewski G, Filip R. Correlation of therapeutic effect of obidoxime and dosing time in the acute intoxication by chlorfenvinphos in rats. Basic Clin Pharmacol Toxicol. 2009 Jul;105(1):37-45. [PubMed Citation]
RePORTER. NIH. Next generation oxime therapeutic for chemical agent inhibited CNS (brain) ChEs.
RePORTER. NIH. Optimization of nonpyridinium oximes for BChE hydrolysis of OPs in plasma.
RePORTER. NIH. Oxime-assisted catalysis of organophosphates and reactivation of AChE.
RePORTER. NIH. Rapid development of in vivo models for countermeasure discovery: organophosphate.
RePORTER. NIH. Synthesis of methylating ligands that reactivate aged acetylcholinesterase.
Rolfsjord LB, Fjaerli HO, Meidel N, Stromme JH, Kowalczyk M, Jacobsen D. Severe organophosphate (demeton-S-methyl) poisoning in a two-year-old child. Vet Hum Toxicol. 1998 Aug;40(4):222-4. [PubMed Citation]
Rubnov S, Shats I, Levy D, Amisar S, Schneider H. Autocatalytic degradation and stability of obidoxime. J Pharm Pharmacol. 1999 Jan;51(1):9-14. [PubMed Citation]
Simon GA, Tirosh MS, Edery H. Administration of obidoxime tablets to man. Plasma levels and side reactions. Arch Toxicol. 1976 Sep 15;36(1):83-8. [PubMed Citation]
Soukup O, Tobin G, Kumar UK, Jun D, Fusek J, Kuca K. Characterization of the anticholinergic properties of obidoxime; functional examinations of the rat atria and the urinary bladder. Toxicol Mech Methods. 2010 Sep;20(7):428-33. [PubMed Citation]
Soukup O, Krůšek J, Kaniaková M, Kumar UK, Oz M, Jun D, Fusek J, Kuča K, Tobin G. Oxime reactivators and their in vivo and in vitro effects on nicotinic receptors. Physiol Res. 2011;60(4):679-86. [PubMed Citation]
Summary of the NIAID Expert Panel Review on Medical Chemical Defense Research, March 19, 2003, Bethesda, MD (NIH/NIAID)
Sweetman SC (ed). Martindale, The Complete Drug Reference. London: Pharmaceutical Press (2009) p.1456
Thiermann H, Mast U, Klimmek R, Eyer P, Hibler A, Pfab R, Felgenhauer N, Zilker T. Cholinesterase status, pharmacokinetics and laboratory findings during obidoxime therapy in organophosphate poisoned patients. Hum Exp Toxicol. 1997 Aug;16(8):473-80. [PubMed Citation]
Thiermann H, Szinicz L, Eyer P, Felgenhauer N, Zilker T, Worek F. Lessons to be learnt from organophosphorus pesticide poisoning for the treatment of nerve agent poisoning. Toxicology. 2007 Apr 20;233(1-3):145-54. [PubMed Citation]
Thiermann H, Zilker T, Eyer F, Felgenhauer N, Eyer P, Worek F. Monitoring of neuromuscular transmission in organophosphate pesticide-poisoned patients. Toxicol Lett. 2009 Dec 15;191(2-3):297-304. [PubMed Citation]
Thiermann H, Eyer F, Felgenhauer N, Pfab R, Zilker T, Eyer P, Worek F. Pharmacokinetics of obidoxime in patients poisoned with organophosphorus compounds. Toxicol Lett. 2010 Sep 1;197(3):236-42. [PubMed Citation]
US NLM. ChemIDplus Lite. Obidoxime
Vos EM, Hens JJ, Lau HS, Boon ES, Bartelink AK. Poisoning with organophosphate compounds. Ned Tijdschr Geneeskd. 2002 Jan 5;146(1):34-7. {PubMed Citation]
Worek F, Aurbek N, Koller M, Becker C, Eyer P, Thiermann H. Kinetic analysis of reactivation and aging of human acetylcholinesterase inhibited by different phosphoramidates. Biochem Pharmacol. 2007 Jun 1;73(11):1807-1817. [PubMed Citation]
Worek F, Aurbek N, Wetherell J, Pearce P, Mann T, Thiermann H. Inhibition, reactivation and aging kinetics of highly toxic organophosphorus compounds: pig versus minipig acetylcholinesterase. Toxicology. 2008 Feb 3;244(1):35-41. [PubMed Citation]
Worek F, Aurbek N, Wille T, Eyer P, Thiermann H. Kinetic analysis of interactions of paraoxon and oximes with human, Rhesus monkey, swine, rabbit, rat and guinea pig acetylcholinesterase. Toxicol Lett. 2011 Jan 15;200(1-2):19-23 [PubMed Citation]
19. Web sites
NIH CounterACT Program (HHS/NIH)
NIH RePORTER (HHS/NIH)
ClinicalTrials.gov (HHS/NIH)
PubMed (HHS/NIH)
DailyMed (HHS/NIH)
Record last updated 1/2/2013